Alpha-1 Antitrypsin Deficiency in COPD and Asthma: Review
Alpha-1 Antitrypsin Deficiency: Review & Update More PulmCCM Topic Updates
Alpha-1 antitrypsin deficiency is underrecognized and by implication undertreated. But many people with alpha-1 antitrypsin deficiency are asymptomatic and will never develop significant emphysema, and the benefits of antiprotease replacement therapy are still unknown. Should you routinely test your patients with chronic obstructive pulmonary disease (COPD) for alpha-1 antitrypsin deficiency? And once the diagnosis is made, should you treat your patients with alpha-1 antitrypsin deficiency with intravenous replacement therapy?
Epidemiology of alpha-1 Antitrypsin Deficiency
There are an estimated 200 to 500 cases of alpha-1 antitrypsin deficiency per million people, and an estimated 70,000 people with the PI*ZZ genotype (homozygous, associated with severe antiprotease deficiency) living in the U.S. Alpha-1 antitrypsin deficiency is underrecognized: only 10,000 people are receiving alpha-1 antitrypsin replacement therapy in the U.S., and most people with known A1ATD report a delay of several years between first presentation and recognition of A1ATD.
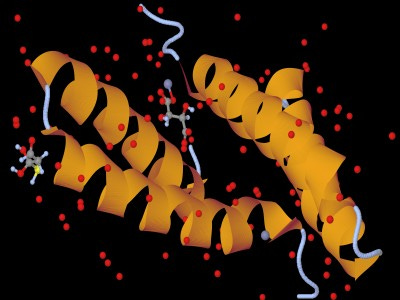
Pathogenesis of alpha-1 Antitrypsin Deficiency
Alpha-1 antitrypsin is an antiprotease made in the liver that protects the lung from damage by ordinary enzymes such as neutrophil elastase. The Z allele is responsible for 95% of cases of alpha-1 antitrypsin deficiency. Decreased alpha-1 antitrypsin levels/function can result in proteolytic damage to the lung (emphysema), or excess polymerization can deposit in and damage tissues (liver disease, and possibly panniculitis and vasculitis). 11 micromoles per liter (80 mg/dL) of alpha-1 antitrypsin is the critical threshold serum level below which emphysema risk increases.
Diagnosis of alpha-1 Antitrypsin Deficiency
Diagnosis is made by checking the serum level of alpha-1 antitrypsin; experts also recommend checking genotype for levels < 100 mg/dL. Free, at-home confidential testing is available (which, notably, is subsidized directly or indirectly by makers of A1AT augmentation therapy products). Expert societies have recommended checking almost routinely, in virtually everyone with COPD, and many people with asthma, for A1ATD.
Clinical Features of alpha-1 Antitrypsin Deficiency
Most patients present with "typical" COPD, both by clinical features and radiography. Panacinar emphysema would generally only be detected on biopsy. Only a minority of people with COPD and severe alpha-1 antitrypsin deficiency have basilar-predominant emphysema (~20% in one series); 36% had apical emphysema in another series. Many cases of COPD due to alpha-1 antitrypsin deficiency are mistaken for ordinary COPD. This may be because people with emphysema due to alpha-1 antitrypsin deficiency are frequently also smokers.
Severe alpha-1 antitrypsin deficiency does not mean COPD will develop, unless the person also smokes (there is a >90% prevalence of COPD in people with severe A1ATD who smoke, but only ~65% of those with PI*ZZ who do not smoke). Most interestingly, asymptomatic, never-smoking people with PI*ZZ and severe alpha-1 antitrypsin deficiency (discovered through screening) had a normal life expectancy in screening studies. Rates of FEV1 decline vary widely, and estimates are so wide as to be meaningless (between 23-316 mL / year in PI*ZZ homozygotes with severe A1ATD).
Treatment of alpha-1 Antitrypsin Deficiency
The usual treatments for COPD are recommended (bronchodilators, exercise, etc). Several commercial preparations of A1AT intravenous replacement therapy are available; they must be given weekly to maintain adequate levels and cost about $100,000/year. Whether to treat any individual patient with intravenous replacement therapy is a difficult question, because the evidence is mixed and suggests many or most patients will not benefit:
Observational studies are conflicting and inconsistent, but by "cherry-picking" between studies, one can infer both a mortality reduction and a slowing of FEV1 decline in the cohorts receiving replacement therapy (which were non-randomized), particularly for people with FEV1 between 35 and 50% predicted.
However, the only 2 randomized trials performed [1, 2] showed no improvement in patient-important outcomes like dyspnea, exacerbations or FEV1 decline (notwithstanding isolated, clinically unimportant findings like lung density on CT scan). They were underpowered/under-followed-up to answer questions of survival benefit.
Still, major societies (ATS, ACCP, ERS, etc) recommend "the selected use of augmentation therapy" in people with emphysema and the PI*ZZ genotype, with bias toward use in those with FEV1 35-60% predicted. Augmentation therapy should not be given to asymptomatic people with the PI*ZZ genotype, nor for people with PI*MZ and COPD (they almost never have A1AT levels < 11 micromoles). PI*SZ people occasionally have A1AT levels < 11; they may be considered for augmentation therapy, although they weren't represented in these (equivocal) trials. Although it's made from pooled human plasma, augmentation therapy has been safe in clinical trials and small postmarketing registries.
Diagnosing and treating everyone in the U.S. with PI*ZZ, severe A1AT deficiency and emphysema would cost an estimated additional $1.5 billion per year (assuming there are 60,000 undiagnosed, 15,000 of them have COPD, and therapy costs $100K / year).
Clinical Takeaway: Alpha-1 antitrypsin deficiency is underrecognized, although not a public health crisis. Increased screening for A1ATD in patients with COPD would certainly result in increased detection, identifying some people who will gain a benefit from augmentation therapy (which for most, would be expected to be slight, based on clinical trial outcomes), along with many more who will not benefit. Some patients might feel better knowing they have alpha-1 antitrypsin deficiency, and that might help them quit or avoid smoking, which could save lives.
Read more:
Alpha1-antitrypsin (AAT) review. Nature Reviews. July 28, 2016.
Alpha1-antitrypsin (AAT) review. Stockley RA. Clin Chest Med. 2014 Mar;35(1):39-50. doi: 10.1016/j.ccm.2013.10.001. Epub 2013 Dec 12.
Stoller JK. Alpha1-antitrypsin (AAT) deficiency review. AJRCCM 2012.


