Atrium Health and UPenn test pressuring doctors to offer more comfort care
Nudge. Nudge. Nudge. Nudge. Nudge. Nudge. [BRICK THROUGH SCREEN]
Academics from the University of Pennsylvania have been teaming up with Big Hospitals to perform research on clinical operations.
The two highest-profile papers we’ve seen so far have both been conducted at massive health systems, focused on limiting care deemed low-value near the end of life.
Both initiatives directly threaten physician autonomy, and in neither do the motivations of the health systems appear likely to be purely “patient-centered.”
In one (Courtright et al, JAMA 2024), the researchers and health system administrators persuaded multiple hospitals’ Medical Executive Committees to sign off on the implementation of automatic palliative care consults on hospitalized patients meeting a certain profile, to see if they reduced length of stay. The consults were “pre-ordered” (note: this is not a thing), with the physician simply informed via pop-up that the consultation had been already ordered on her patient. Canceling it required a separate discontinuation order and a written explanation.
This took place at 11 hospitals owned by Ascension, a $27 billion, 140-hospital conglomerate operating in 19 states—the third-largest system in the U.S by some accounts (after HCA and the VA).
The automatic consults overwhelmed the hospitals’ palliative care services and had little effect overall. We covered that here:
Automated palliative care consults: is this a good idea?
Palliative care programs are sometimes pitched to administrators on the basis of their potential to reduce costs, by shortening length-of-stay or intensity of expensive and unhelpful therapies at the end of life. Observational data suggests palliative care consultation
UPenn’s next dance was with North Carolina’s Atrium Health, which was then only a piddling $10 billion operation with 40 hospitals throughout the South, paying its CEO a mere $9.8 million in 2021, according to Axios. In a scathing report, N.C. state treasurer Dale Folwell said Atrium “has prioritized the paychecks of its top executives over its charitable mission.”
Atrium filed 2,482 lawsuits against patients with medical debt between January 2017 and June 2022, the most of any system in the state, Duke legal researchers reported. Atrium benefited from North Carolina’s 8% interest rate on unpaid debts, with interest charges comprising one-third of the $57 million collected by all health systems during that time, according to the Duke authors.
Then Atrium merged with Midwest-based Advocate Aurora Health in 2022 to become one of the largest health systems in the U.S.
After the merger, the nonprofit’s executives raised their pay by an average of 41% for 2024, according to North Carolina Health News and The Charlotte Ledger.
But wait. That’s all off-topic…. or is it? And wasn’t there a research paper in here somewhere?
Offer Comfort Care or Tell Me Why Not
Aided by UPenn academics, Cerner coding gnomes at Atrium created and launched an EMR popup that fired every time the attending ICU physician placed an order, demanding the doctor estimate the patient’s risk of death and implicitly pressuring her to offer comfort care to patients for whom the algorithm predicted a short life expectancy or perceived low quality of life.
They didn’t call it pressure, though. They called it a “nudge.” Just a friendly little nudge, that’s all.
The friendly nudging pop-up fired on all ICU patients vented for ≥48 hours with a preexisting “serious illness,” including chronic obstructive pulmonary disease, heart failure, interstitial lung disease, cirrhosis, dementia, kidney failure, solid cancer, leukemia, or lymphoma.
According to the methods, they didn’t go through the MECs on this study. The IRBs approved it, waiving informed consent. Then it rolled out in a stepped-wedge cluster randomized trial at 17 ICUs at 10 hospitals.
When the algorithm found a vented patient with a “serious illness,” it fired a popup that looked something like this:
Hard to argue with this one on its own. Maybe being forced to consider this on every patient at high risk for poor outcomes would be a good idea.
But then they went here:
This fired (apparently, from the methods) on every patient with COPD, heart failure, renal failure, or limited-stage cancer, at any age, who was vented for 2 days (in two of the 4 arms of the study).
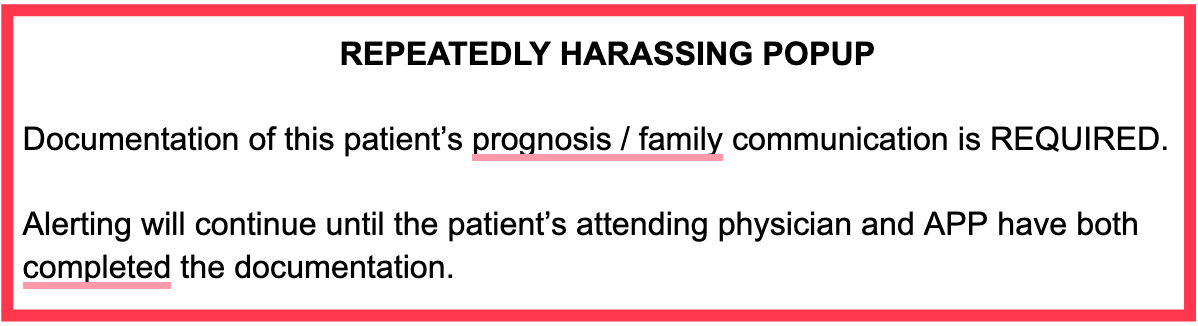
If the physician or APP declined to participate, they would both get to see this friendly nudge:
And again.
And again. Every time they placed an order.
Hey, all you have to do to make it go away is answer my questions. You gotta problem with that? What. You don’t wanna answer my questions? Okay. That’s okay. I’ll ask you again in five minutes.
…
Hey. Me again. What, you don’t like comfort care? You don’t like people to be comfortable? You want them to be uncomfortable? Just explain it to me. ‘Splain it to me so I understand.
They did this in 4 arms, so sites would either have no popups, one of the two, or both.
Results
Data was reported from 3,250 patients who were an average age of 63.
One-quarter were younger than 57 years old.
Have you offered the option of care primarily focused on comfort (including withdrawal of life support) to your 50-year-old patient? Why not? Provide a justification. Others will see your response.
Care teams had an impressive 25% rate of defiance, I mean, the intervention document non-completion rate.
Also,
More patients who were “double-popped-up” (the so-called combination group) were discharged to hospice (8.9% vs 7.3% in the “no-popup” patients).
Comfort care orders were placed an average of one day earlier in the patients whose physicians were pressured to do so (3.6 days vs 4.5 days).
There was no difference in vent duration, use of CPR, ICU length of stay or mortality or readmission, mortality at 30, 90, or 180 days, or multiple other secondary outcomes.
Or as the authors put it more succinctly,
“The prognosis intervention did not impact any end-of-life processes or outcomes.”
What were the effects on physician morale, or on the physician-patient-family relationships? Well … Um. Those are hard to study, you know?
Funding
The Donaghue Foundation funded the study, not Atrium Health, according to the authors.
The foundation’s website states they “prioritize the development of solutions to combat the symptoms of low-value care.”
In its Another Look grant program, the website lists its first priority as “improving the quality and availability of palliative, end of life, and hospice care.”
Discussion
Here we have a morbidly fascinating mixture of some of the insidious processes at work in U.S. healthcare today: increasing corporatization and consolidation of financialized “non-profit” health systems; the co-optation of palliative care as a potential cost-saving instrument, rather than for actual palliation of suffering; a steady reduction of physician autonomy with increasingly brazen control over (employed) physician behavior to pursue organizational goals, with the use of the EMR as the primary instrument of control.
The new twist here is the eager participation by Ivy League academics in the enterprise, under the aegis of philanthropically funded research.
Enhancing our consideration of critically ill patients’ prognoses and flagging those who might benefit most from additional goals-of-care discussions are important and legitimate efforts.
Forcing physicians to participate against their will in a poorly-designed study that commandeers their massive corporate employer’s EMR to pester and harass them, supplanting their judgment with the simplistic, arrogant, and false assumption that every patient with COPD or heart failure or prostate cancer vented for 2 days should be considered for withdrawal of life support, and powering it all with an implicit threat of negative professional judgment by their administrative bosses who have already shown their moral compass and true feelings for their patients and neighbors by suing the shit out of them, is just an unfortunate way to see things turn.
And after all that, a few more patients got discharged to hospice, a day sooner.
Physicians should push back on any attempt at expanding or replicating this misguided venture.
But don’t call it pushback. Just call it a friendly nudge.







This is unconscionable. The purpose of palliative care is not of fulfill some administrator or researchers notion of what high value care means, and especially not to shorten length of ICU or hospital stay. I can imaging that administrators greedily agreed to these EMR modifications, and the sad part is that it isn't even difficult to imagine. Think of the administrators you know personally and ask yourself if you think they'd have any difficulty with it. Think of the physician and APP partners you work with and ask yourself if THEY would have any difficulty with it. Enough said. The purpose of palliative care is to provide comfort and human kindness to those human beings for whom we can't provide cure.
Our enterprise, which is human in its roots and its essence, is being hacked away at by counters of beans and guardians of "efficiency", and the tree is near to being felled. We ceded them the authority, handed them the axe, decades ago, and our patients pay the price. In every sense of the phrase. I fear both for our patients and for what it means to be a human physician in the coming age of AI. Several papers now show that machines can seem more empathetic to patients than their doctors do. Imagine that technology in the hands of those seeking "enterprise efficiency", the mantra of those who don't grok why we are here and seek only more dollars on the mountain of them and more hospitals in the collection.
The thread I have to hang on to is only this: machines can sound empathetic, but they can never, ever HAVE empathy. We must constantly work at showing ours. Empathy over efficiency. Knowledge over stored data. Wisdom over activity. Human kindness over all. That is the essence of medicine. When we wander from that we lose our purpose.
Good Lord. Big Brother is indeed watching. I can not think of a better way to make physicians mad and NOT cooperate.
I absolutely believe in appropriate Palliative Care consults, but the consultants need to be well trained, adequately staffed and have good social skills. This is often not the case.
Luckily, where I practice, we have a tremendous PC team and I involve them ASAP. I could care less about LOS and dollars saved. Its about human beings looking out for each other.