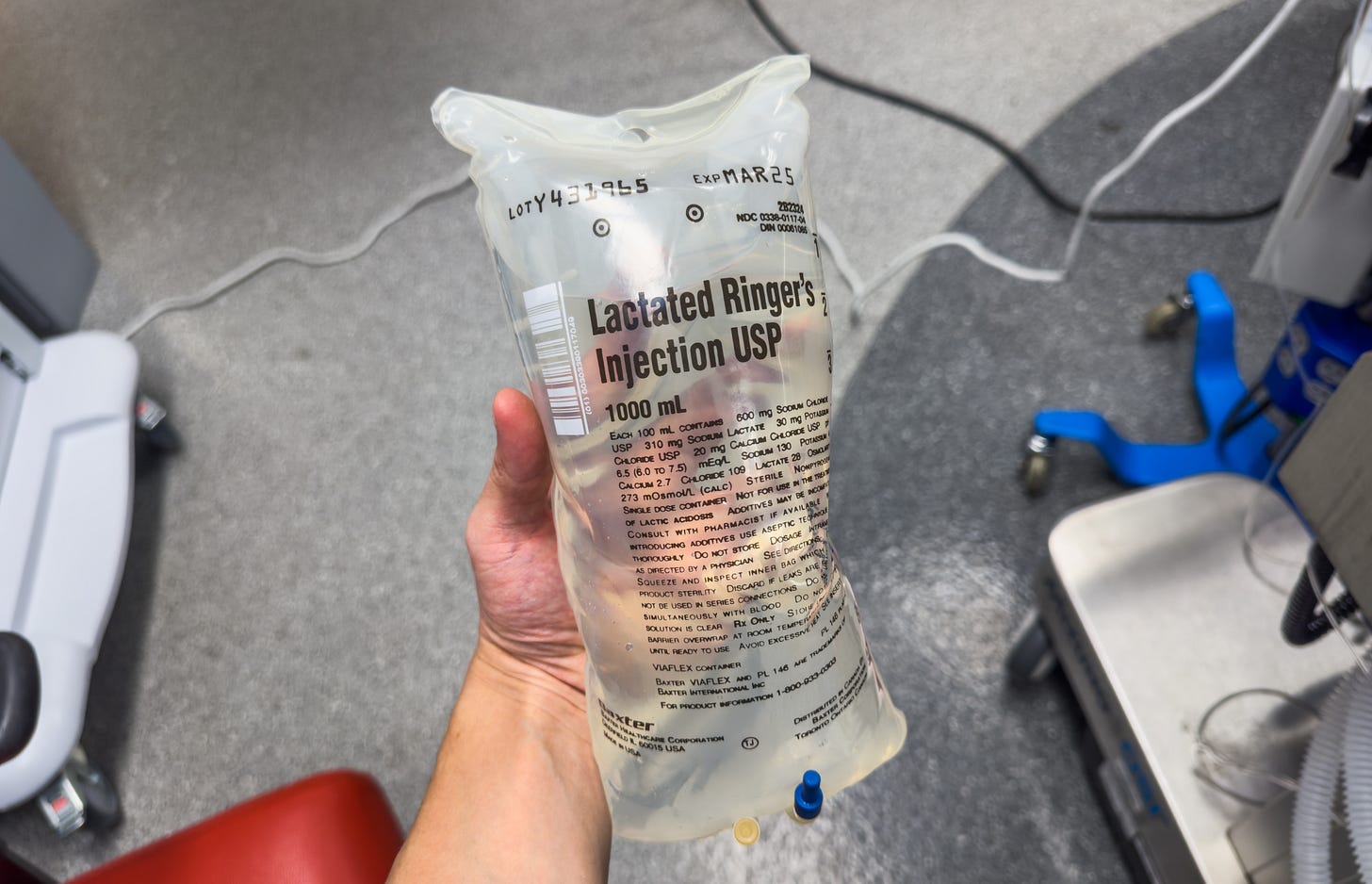
Balanced solutions vs saline (FLUID trial)
Does lactated Ringer's save lives in the ICU, or not?
The massive, biggest-ever randomized FLUID trial (McIntyre et al, NEJM 2025) found no difference in mortality between patients treated with normal saline and balanced crystalloid solutions (lactated Ringer’s).
But critical care societies have advised infusing balanced solutions in patients with sepsis and critically ill patients generally, based on prior randomized trial data. Does FLUID refute that guidance?
FLUID Trial
FLUID enrolled over 53,000 patients at seven hospitals in Ontario, Canada from 2016 to 2020. Sixteen sites were originally planned, with enrollment truncated due to the Covid pandemic (43,600 patients had complete data and were analyzed).
After about 15 weeks using one fluid type, each entire hospital flipped randomly to the other (saline to lactated Ringer’s or vice versa) in an unblinded (open-label), cluster-randomization design. They then used the other fluid for 15 weeks.
Few patients in FLUID were critically ill. Most were in the emergency department and hospital wards, with ~25% admitted for elective surgery and only about 15% admitted to the ICU.
Some hospitals tended not disregard the protocol. Adherence with the LR portion of the protocol was only 78%.
Adherence meant stocking at least 80% of the fluid inventory with the target fluid. Clinician orders for the off-target fluid were set to automatically convert to the target fluid. Thus, this was a trial of an administrative intervention as much as a clinical one.
The data was collected at the administrative level, without providing the more granular detail of patient-level data.
Results
At 90 days of follow-up, death/readmission occurred in 20.3% of patients randomized to LR, and 21.4% of normal saline patients. This was statistically nonsignificant.
Death occurred in 6.9% of the LR patients vs. 7.6% of the saline-assigned patients (RR 0.97, CI 0.89 to 1.07).
Dialysis occurred with equivalent frequency between groups (0.5% vs 0.6%).
One major strength of FLUID’s design was that it captured all fluid administration before arrival in the ICU, which was a criticism of some earlier studies.
However, FLUID’s interrupted enrollment due to the pandemic, combined with the small expected difference (≤1% absolute) between fluid strategies, meant it was likely underpowered to detect a difference.
FLUID vs Prior Trials
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.