Blood transfusion targets in acute brain injury: Review (Updated)
Are brain injuries an exception to the "less is more" heuristic in transfusion during critical illness?
This review was first published in October 2024; it is updated here with important new results from the SAHARA trial (English et al NEJM 2024), with a series of (rough) meta-analyses of recent data. -Ed.
When deciding whether to transfuse red blood cells to critically ill patients with anemia, less is more, generally speaking.
Because transfusion can be harmful, current practice is to usually restrict it in the ICU to patients with hemoglobin less than 7 g/dL. Some patients, though (e.g., those with significant coronary artery disease), may benefit from higher transfusion thresholds.
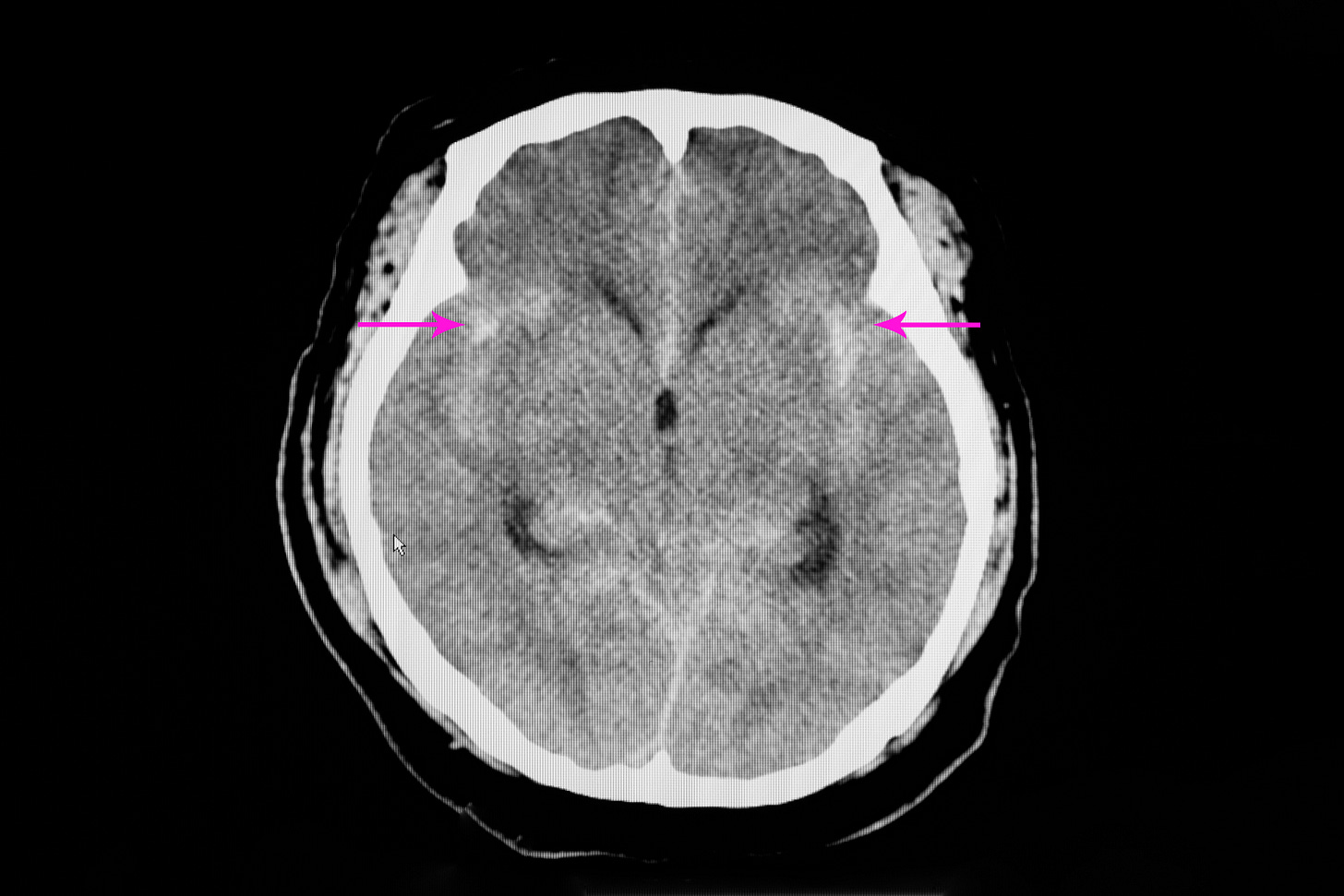
Brain-injured patients, including those with traumatic brain injury (TBI) and hemorrhagic strokes, were not well-represented in randomized trials studying transfusion thresholds in critical illness. Anemia—or transfusion—might be more harmful to injured brains than non-injured ones, for various reasons.
Three randomized trials published in 2024 provide some evidence to inform transfusion decisions in brain-injured patients, although the trials suffer from possible underpowering and (in one) aggregation of unalike patients.
Here we’ll look at each trial in turn and combine them in two improvised meta-analyses.
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.