Cardiogenic Shock (Research Review)
Impellas changed the game for MI-related shock. What else is new?
This is a research review and clinical update on cardiogenic shock, initially published January 19, 2026. This review will be periodically updated; its publication reflects the date of its most recent update. -Ed.
When the heart fails—really fails, far beyond that inaptly-named chronic condition called “heart failure” that people live with for decades—it’s a big, bad problem.
In cardiogenic shock, critically impaired cardiac function leads to low blood pressure leads to low tissue perfusion leads to reduced blood return leads to reduced coronary artery perfusion further reducing cardiac contractility … and on around again, until either the terrible cycle is somehow interrupted, or multiorgan failure occurs (potentiated by tissue ischemia, inflammation, and worsened hypotension from peripheral vasodilation), and too often death.
Even with excellent treatment, mortality from cardiogenic shock still approaches 50% at 30 days. Cardiogenic shock remains the most common cause of death for patients with myocardial infarction.
The management of cardiogenic shock continues to be dominated by convention and clinical experience, as almost all commonly used interventions lack robust supporting evidence from randomized trials.
New treatments—namely, the microaxial flow pump (Impella™) haven’t significantly improved overall survival, but can be lifesaving in some patients.
Cardiogenic Shock Overview
Shock has been defined clinically as systolic blood pressure <90 mm Hg for a sustained period (e.g., 30 minutes) or a need for vasoactive agents to maintain that pressure, along with evidence of systemic hypoperfusion (e.g., cool extremities, lactatemia, encephalopathy, oliguria) and evidence of cardiac dysfunction on echocardiogram.
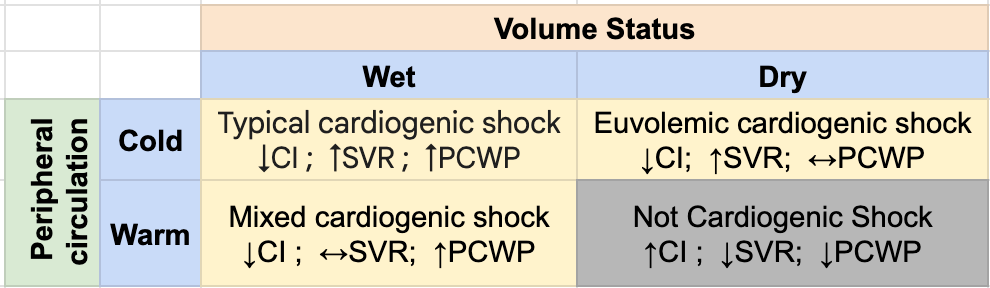
Low cardiac output (cardiac index ≤2.2 L/min/m2 ) and high systemic vascular resistance (>2200 dynes/cm/sec) are common in classic presentations, and (when measurements are available) can help differentiate cardiogenic shock from distributive (e.g., septic) or other forms of shock.
The age-old 2x2 schema categorizing shock patients by volume status and peripheral circulation is still relevant and applicable to cardiogenic shock patients:
Staging systems have been proposed, which rely in part on subjective interpretation of clinical status; they may add little to bedside clinical assessment and don’t provide reliable prognostic data at the patient level, but are commonly used in research settings and specialized cardiac care centers. The SCAI’s model, with grades severity from A (at risk) to E (in extremis) is in the widest use.
MI-related Cardiogenic Shock
Historically, ST-elevation MI was responsible for the majority of cardiogenic shock, and STEMIs still cause a large proportion of cases. Immediate revascularization is the cornerstone of therapy.
Microaxial flow pumps (Impella™) represent the single most significant recent advance in management for cardiogenic shock. Impella (the only such device available) is supported in U.S. guidelines for its potential to save lives in selected patients with shock after acute STEMI, despite a significant risk of device-related complications.
Impella saves lives in STEMI with shock, but with major risks (DanGer Shock)
Patients with acute ST-elevation myocardial infarction with cardiogenic shock treated with the Impella CP flow pump for mechanical circulatory support had increased survival at 6 months compared to those receiving standard care, the DanGer Shock randomized trial showed
More data on Impella complications emerge
The DanGer-Shock randomized trial allowed interventional cardiologists to breathe a bit easier, knowing that the Impella device resulted in improved survival 6 months after ST-elevation myocardial infarction with cardiogenic shock:
Non-MI-related Cardiogenic Shock
With improved systems of care delivery and cardiovascular prevention, MI has been declining as an etiology. Increasingly common today are new onset or acute-on-chronic heart failure, mixed shock states, and postcardiotomy syndrome after cardiac surgery.
Arrhythmias (e.g, atrial fibrillation), new or worsening valvular disease, pericardial disease, medication nonadherence, excess fluid or sodium intake, obesity hypoventilation syndrome, drug and alcohol use, pulmonary embolism, post-cardiac arrest stunning, infections, and other causes must be considered in cases of non-MI-related cardiogenic shock.
Owing to the absence of reliable evidence to guide management in patients with non-MI-related cardiogenic shock, management tends to be clinician- and center-dependent.
Observational evidence suggests that patients treated at advanced cardiac centers (including most tertiary hospitals) have better outcomes.
Cardiogenic Shock Management: Culture, Convention, Controversy
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.