Inspiratory collapse of the inferior vena cava: What is it telling us?
ICU Physiology in 1000 Words by Jon-Emile Kenny
Thousands of subscribers have joined PulmCCM since Jon-Emile Kenny wrote regularly for the publication. We’ll share one of his always insightful, occasionally inscrutable posts from time to time. I think they’ve aged very well, as has Jon. Enjoy! -Matt
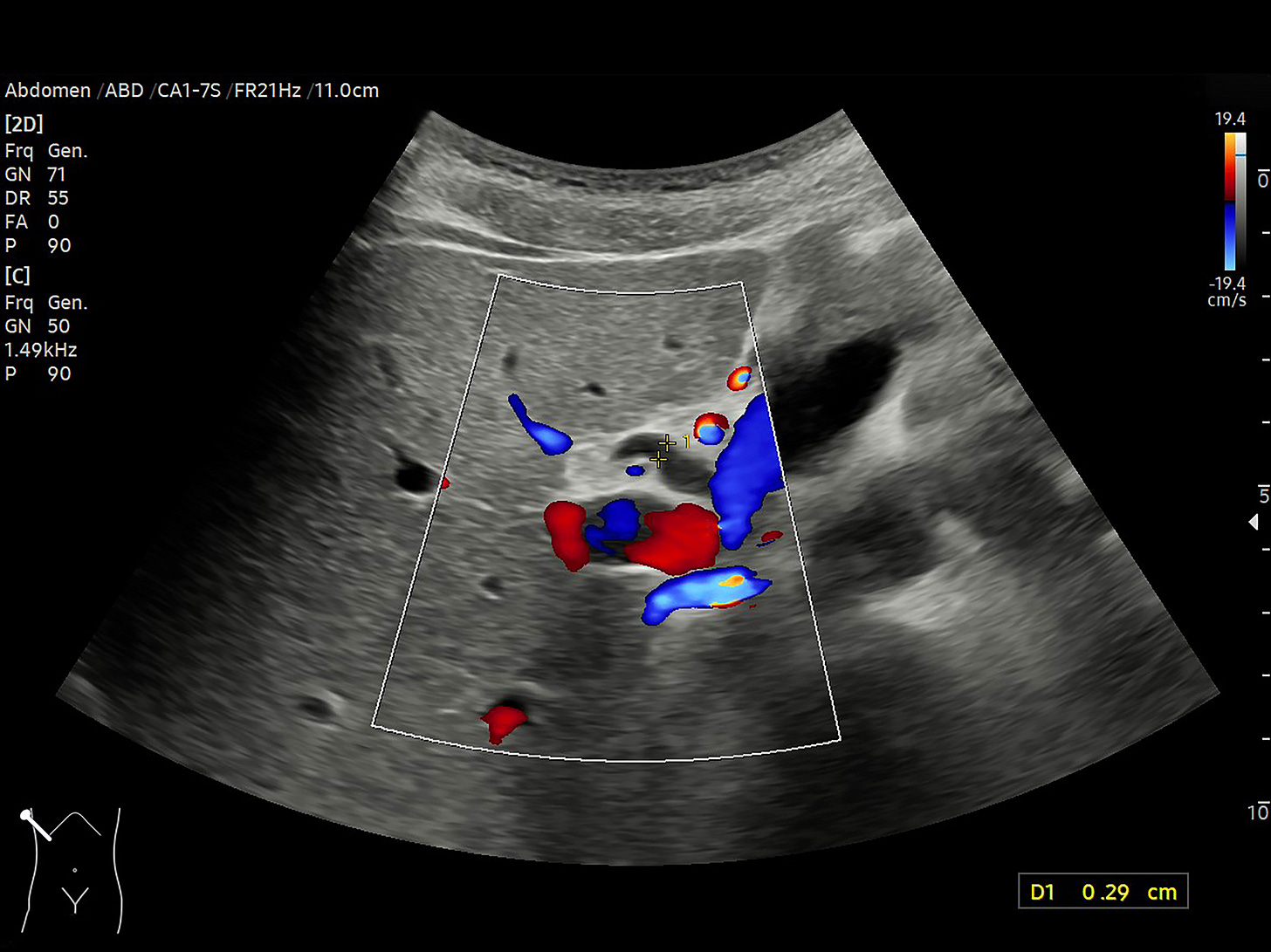
With the dissemination of small, portable, ultrasound devices [or SPUDs], it seems that it is every house-officer’s dream to own the ability and wherewithal to place an ultrasound probe on a patient and find something meaningful; but what exactly is inferior vena cava [IVC] collapse with inspiration telling us?
The reason IVC collapse occurs is that a Starling Resistor is generated — when the pressure within a distensible tube drops below the pressure without the tube. It seems straightforward, therefore, that collapse depends on two competing pressures:
The pressure within the IVC which is related to the central venous pressure [CVP, i.e. the right atrial pressure barring any caval obstruction] and
The pressure within the abdominal cavity.
Collapse of the IVC will be facilitated by a diminution of 1.], an augmentation of 2.], or a combination of both. Addressing each of these forces in turn:
1. Pressure within the Inferior Vena Cava
Why does the pressure within the IVC decrease with a spontaneous inspiration? The right atrium is a thin-walled, compliant structure and the pressure within the right atrium falls with the pleural pressure during a spontaneous inspiratory effort. This drop in CVP is transmitted down the IVC. The degree to which the CVP falls during spontaneous inspiration depends upon three competing variables:
The drop in pleural pressure, as above
Venous return function, and
Cardiac function.
This should make intuitive sense - the pressure within the right atrium during spontaneous inspiration will be influenced by the pleural pressure tending to pull the CVP down, the venous return from the lower body tending to push the CVP up and the cardiac function ejecting blood from the thorax, also tending to push the CVP down. This physiology is best understood by analysis of the Guyton diagram which overlays venous return and cardiac function onto a single graph. The intersection of the two curves defines the operating point of the cardiovascular system – the pressure at which this occurs is the central venous pressure. A drop in pleural pressure is depicted by shifting the cardiac function curve leftwards with respect to the venous return curve [1].
But does this inspiratory reduction in central venous pressure tell us anything definitive about a patient’s ‘volume status’ [i.e. whether the patient is euvolemic or not] or ‘volume responsiveness’ [i.e. whether the patient will augment his or her cardiac output with fluid administration]? Unfortunately, no [2-7]. The reason is that the central venous pressure is dependent upon the intersection of venous return and cardiac function – two physiological phenomena each with multiple determinants. ‘Volume status’ plays a role in venous return in that hypovolemia tends to decrease venous return and therefore, CVP, but venous return has other determinants. This also explains the lack of relationship between volume status and CVP [5]. ‘Volume responsiveness’ is determined by how far the operating point is from the plateau of the cardiac function curve. Because the slope of the cardiac function curve is hard to know with certainty, almost any CVP may fall upon the plateau, especially in patients with cardiac abnormalities [e.g. those in the intensive care unit] [8].
2. Pressure within the Abdominal Cavity
Complicating matters is the increase in abdominal pressure which facilitates IVC collapse. Because positive end-expiratory pressure, intra-abdominal hypertension and breathing pattern all affect the degree of abdominal pressurization [9-12], IVC collapse can be confounded. Thus, inspiratory IVC collapse tells us that the CVP is falling below the intra-abdominal pressure. If there is no pathogenic or iatrogenic pressurization of the abdomen [e.g. PEEP, auto-PEEP, ascites], and inspiration is not stressed [e.g. dyspnea, breathing through an endotracheal tube], then IVC collapse tells us that the CVP is low. The clinician must then understand that a low CVP may be the result of:
Hypovolemia,
High resistance to venous return [e.g. alpha agonist effects],
High venous compliance [e.g. venodilators, sepsis], and
Hyper-dynamic cardiac function [e.g. extrinsic or intrinsic adrenergic tone].
These caveats remind us that notwithstanding the occasional high utility of inspiratory IVC collapse as a clinical measurement, there is no such thing as a silver bullet in the assessment of volume status, volume responsiveness, and vascular tone.
For a 2017 update on this topic, please read this post.
Check out other articles in this series,
Read more from Jon-Emile Kenny on his website at Heart-Lung.org.
References:
1. Magder, S., Bench-to-bedside review: An approach to hemodynamic monitoring - Guyton at the bedside. Crit Care, 2012. 16(5): p. 236.
2. Muller, L., et al., Respiratory variations of inferior vena cava diameter to predict fluid responsiveness in spontaneously breathing patients with acute circulatory failure: need for a cautious use. Crit Care, 2012. 16(5): p. R188.
3. Corl, K., A.M. Napoli, and F. Gardiner, Bedside sonographic measurement of the inferior vena cava caval index is a poor predictor of fluid responsiveness in emergency department patients. Emerg Med Australas, 2012. 24(5): p. 534-9.
4. Bodson, L. and A. Vieillard-Baron, Respiratory variation in inferior vena cava diameter: surrogate of central venous pressure or parameter of fluid responsiveness? Let the physiology reply. Crit Care, 2012. 16(6): p. 181.
5. Shippy, C.R., P.L. Appel, and W.C. Shoemaker, Reliability of clinical monitoring to assess blood volume in critically ill patients. Crit Care Med, 1984. 12(2): p. 107-12.
6. Marik, P.E. and R. Cavallazzi, Does the central venous pressure predict fluid responsiveness? An updated meta-analysis and a plea for some common sense. Crit Care Med, 2013. 41(7): p. 1774-81.
7. Kumar, A., et al., Pulmonary artery occlusion pressure and central venous pressure fail to predict ventricular filling volume, cardiac performance, or the response to volume infusion in normal subjects. Crit Care Med, 2004. 32(3): p. 691-9.
8. Magder, S. and F. Bafaqeeh, The clinical role of central venous pressure measurements. J Intensive Care Med, 2007. 22(1): p. 44-51.
9. Fessler, H.E., et al., Effects of Positive End-Expiratory Pressure on the Gradient for Venous Return. American Review of Respiratory Disease, 1991. 143(1): p. 19-24.
10. Lloyd, T.C., Jr., Effect of inspiration on inferior vena caval blood flow in dogs. J Appl Physiol Respir Environ Exerc Physiol, 1983. 55(6): p. 1701-8.
11. Rubinson, R.M., et al., Inferior Vena Caval Obstruction from Increased Intra-Abdominal Pressure - Experimental Hemodynamic and Angiographic Observations. Archives of Surgery, 1967. 94(6): p. 766-&.
12. Kimura, B.J., et al., The effect of breathing manner on inferior vena caval diameter. European Journal of Echocardiography, 2011. 12(2).