Inferior vena cava filters are overused. What's the harm?
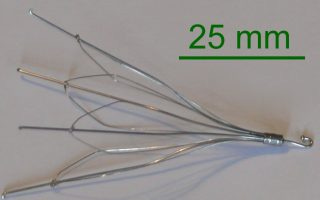
image: Wikipedia Inferior vena cava filters (IVCF) are placed to prevent deep venous thromboses (DVT) from traveling to the heart and lungs, causing pulmonary embolism (PE). IVC filters' rationale makes sense, but despite their wide use, the benefits and risks of IVCF remain unclear. With about 50,000 IVC filters placed annually in the U.S., that's a lot of unclarity. IVCF are standard care for patients with acute pulmonary embolism or proximal DVT who cannot receive anticoagulation because of bleeding risk. But IVCF are used more often as an additional preventive therapy along with anticoagulation in an attempt to further reduce PE risk. Is this good medicine?
Evidence for Benefits of IVC Filters is Low
The evidence supporting the use of IVCF for any indication is low. Two large randomized trials have been performed; neither showed a mortality reduction from IVC filters: In PREPIC (1998) and its 8-year follow up study, patients with either DVT or PE receiving IVCF had fewer recurrent PEs, but got more DVTs and had no reduction in mortality. PREPIC's design is obsolete today: half its patients had routine DVTs without PE, and its IVCF were nonretrievable. PREPIC's main contribution was to confirm that routine placement of permanent IVC filters in DVT and PE is not a good idea. In the wake of PREPIC, almost all IVCF placed in the U.S. today are retrievable. PREPIC2's (2015) updated design tested retrievable IVCF (with anticoagulation, vs anticoagulation alone) enrolling ~400 'high risk' patients with acute PE. There was no difference in death or recurrent PE between groups at 3 or 6 months. Although closer to real-world practice today, 'high risk' in PREPIC2 included anyone over 75, or with any active cancer diagnosis, which are not widely accepted indications for IVCF. Fewer than 18% of patients in PREPIC2 had any hypotension during their hospitalization. On the other hand, a retrospective review of a large inpatient database did show IVCF placement was associated with improved survival in elderly patients with massive PE (i.e., with hypotension). Unsurprisingly, no randomized trial testing this IVCF indication has been performed.
Professional Societies Disagree on IVC Filter Indications
There are only two indications for IVCF placement that are generally accepted by all major professional societies:
Acute PE or proximal DVT with inability to provide anticoagulation;
Patients with hemodynamically unstable PE, for whom another PE might be fatal.
Beyond that, professional societies disagree on appropriate indications for IVC filters. For example, while the American College of Radiology (ACR) supports prophylactic placement of IVCF in patients with severe trauma or spinal injury without DVT, the American College of Chest Physicians (ACCP) advises against it. On the other hand, ACCP endorses IVCF placement as an adjunctive measure for massive PE treated with thrombolysis*, but American Heart Association (AHA) disagrees. Radiology professional societies, whose members commonly place IVC filters, happen to endorse more IVCF indications than do ACCP and AHA. *ACCP advises against the routine use of IVCF in PE and DVT but adds "our recommendation against insertion of an IVC filter in patients with acute PE who are anticoagulated may not apply to [patients with hypotension]."
Risks of IVC Filters
Most "retrievable" IVC filters become permanent, because less than a third of IVCF are ever removed. Although "patient lost to follow-up" is the frequently cited reason, failure to remove an IVCF is more likely due to inadequate communication and care coordination by physicians between the inpatient and outpatient settings. Another reason might be the general reluctance to remove the supposed protection provided by the IVC filter. No one knows for sure the risks of IVC filters, because there is no comprehensive public repository for adverse events from IVCF. Complications of IVCF placement frequently occur, but the rate of genuine harm is unknown. IVC filters have been considered reasonably safe mainly because hundreds of thousands have been placed without large safety signals emerging. However, a retrospective review of 952 patients after IVCF placement suggested a 1% rate of serious complications from IVCF. After receiving thousands of adverse event reports, the FDA advised physicians to remove IVC filters as soon as feasible--ideally within two months--and demanded additional longitudinal product safety data from manufacturers. The PRESERVE trial is ongoing in response. Class action lawsuits asserting negligence and product defects are pending against at least three IVC filter manufacturers.
What Doctors Owe Patients with IVC Filters
IVC filters are a roughly $200 million business. In the U.S., Medicare pays about $3,800 to put one in and another $2,250 to take it out. Hospitals split the take with the interventional physician (radiologist, surgeon, cardiologist). With all that money sloshing around, and the payment on the table for IVC filter removal, why can't doctors, hospitals and industry at least get organized enough to take them out? Why can't the hospital schedule IVCF removal at the time it's placed, for 60-90 days after the patient leaves the hospital? Why can't the manufacturers maintain a registry and pay a few call center reps, or robots, to politely harass the IVCF recipients by phone, mail, and email, beginning one month after the filter placement? Add $30 to the device cost, and have a FedEx package arrive at the patient's home address 60 days after IVCF placement containing a scary letter and a number to call. As for doctors, guidelines can't cover every patient scenario, and IVC filters haven't been tested in randomized trials in the truly high risk patients with pulmonary embolism. There may be many patients who benefit from IVCF placement slightly outside the ACCP/AHA guidelines. But not the >50% who are currently receiving IVC filters for off-guideline indications. Blaming the patient and primary physician for IVC filters left in place won't cut it anymore. As physicians we owe it to patients to be more mindful about placement of IVC filters, and more responsible about arranging their prompt removal. Read more: Antithrombotic Therapy for VTE Disease, ACCP guidelines. Appropriate Use of Inferior Vena Cava Filters, ACC website Quality Improvement Guidelines for the Performance of Inferior Vena Cava Filter Placement for the Prevention of Pulmonary Embolism, JVIR.


