Nintedanib protects lung function, prevents exacerbations of idiopathic pulmonary fibrosis (INPULSIS)
In 2011 PulmCCM reported the findings of the phase 2 TOMORROW study, showing Boehringer Ingelheim's tyrosine kinase inhibitor code-named BIBF 1120 reduced lung function decline and prevented exacerbations in people with idiopathic pulmonary fibrosis (IPF). At the 2014 American Thoracic Society annual meeting and in the New England Journal of Medicine, investigators announced their latest trial results for the new molecule, now named nintedanib, tested in two large phase 3 randomized trials (INPULSIS-1 and INPULSIS-2):
Nintedanib reduced the decline of forced vital capacity (FVC) by about 100 mL compared to placebo (in both trials), and also prevented IPF exacerbations (in one of the two trials).
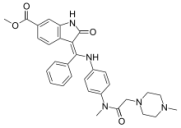
Nintedanib is a tyrosine kinase inhibitor that acts on several targets: vascular endothelial growth factor receptor (VEGFR), fibroblast growth factor receptor (FGFR) and platelet-derived growth factor receptor (PDGFR) — all receptors known to be involved in lung fibrosis. INPULSIS-1 and INPULSIS-2 were conducted at 205 sites in 24 countries, enrolling about 1,000 total patients with a diagnosis of IPF and a forced vital capacity ≥50% predicted along with diffusion impairment. Patients received nintedanib 150 mg b.i.d. or placebo for one year. The rationale for the 2 separate trials was not immediately apparent from the published paper. Some patients also received up to 15 mg prednisone daily if they were taking it at trial enrollment, and if they deteriorated during the trial, their physicians were allowed to treat them with concomitant open-label azathioprine, Cytoxan, N-acetylcysteine, or increased systemic steroid doses. Diarrhea was more commonly reported among study drug participants and about one in 25 stopped nintedanib due to diarrhea. Significant transaminitis was also more common in nintedanib users (~5%, about a 4% excess over placebo). There were also 10 myocardial infarctions among people taking nintedanib, compared to only 2 taking placebo. Nintedanib patients had a significant delay in time to first exacerbation of IPF in INPULSIS-2, and a reduction in the number of patients experiencing IPF exacerbations (4% nintedanib vs. 10% with placebo). This benefit was not seen among patients taking nintedanib in INPULSIS-1, who had no reduction in time to first exacerbation of IPF, nor in the proportion of patients experiencing IPF exacerbations (6% vs 5%). Authors point out that exacerbations of IPF are fairly uncommon events, and infrequent IPF exacerbations in INPULSIS-1 could have precluded any detection of benefit. There was no survival benefit attributable to nintedanib for IPF in the INPULSIS trials, despite a trend toward improved survival among those taking study drug (~6% vs. 8% taking placebo). Along with the exciting results for pirfenidone in ASCEND, the INPULSIS trials for nintedanib could usher in a new era of treatment for IPF, an illness that had remained stubbornly untreatable despite decades of biomedical research and innovation. Pirfenidone's apparent mortality benefit and absence of a cardiovascular safety question may give it the early lead in the new race toward FDA approval and standard-of-care status for these new treatments for idiopathic pulmonary fibrosis. Luca Richeldi et al. Efficacy and Safety of Nintedanib in Idiopathic Pulmonary Fibrosis. INPULSIS trials. NEJM May 18, 2014; DOI: 10.1056/NEJMoa1402584


