Nutrition in severe pancreatitis: none at all (for 3 days) worked fine
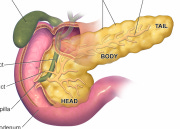
Image: Wikipedia
Acute pancreatitis is a common and usually self-limited illness resolving after a few days of rest and not eating. A minority of people develop severe pancreatitis with necrosis, which can transform pancreatitis into an ordeal lasting weeks or months, characterized by multi-organ failure, infections, and a >15% mortality rate.
Those infections are believed to be caused by translocation of gut bacteria into the bloodstream. Conventional wisdom has it that nutritional strategies can reduce the risk of infection and death in severe pancreatitis, although it's a small evidence base:
Enteral nutrition seems superior to total parenteral nutrition. A 2010 Cochrane meta-analysis of 8 small randomized trials of pancreatitis patients (n=348) showed a 50% risk reduction for death and a 60% risk reduction for systemic infections or need for surgery, favoring enteral nutrition compared to total parenteral nutrition. There was no placebo -- so no way to prove enteric feedings were any better than IV fluids alone -- but TPN was deemed second-line with possible harms, to be used only in those with pancreatitis intolerant of enteral feedings. This analysis examined the route but not timing of nutrition.
Early nutrition (by whatever route) seems better than waiting. A meta-analysis (2009) of non-randomized trials suggested starting enteral feeding within 48 hours was associated with 50-60% reductions in infections and mortality, as compared to delayed nutritional strategies (which could be enteral or parenteral). This analysis addressed timing of nutrition, but not the route.
Ergo, early enteral nutrition became the preferred treatment for severe (necrotizing) acute pancreatitis. For non-severe acute pancreatitis, guidelines advise patients simply not eat for 5-7 days until symptoms subside. One problem, however, has been prognosticating who will progress to severe pancreatitis -- at which point, days later, the opportunity for "early" nutrition has passed.
Is Early Enteral Nutrition in Severe Acute Pancreatitis Needed?
A study in the New England Journal of Medicine helps address that dilemma, while raising its own questions whether an early enteral nutrition strategy is in fact necessary or helpful in all patients with severe acute pancreatitis.
In the PYTHON study, 208 patients with severe acute pancreatitis at 19 Dutch hospitals were randomized to either undergo:
Nasojejunal feeding tube placement a.s.a.p., with enteral feedings started within 24 hours of randomization, or
No nutrition at all for 3 days. Only intravenous fluids were given (unless the patient asked for something to eat) for 72 hours, after which a nasojejunal feeding tube was placed and enteral feedings were started if needed.
Patients were ill, with mean APACHE scores of 11, two-thirds showing signs of SIRS/sepsis, and ~10% ultimately experiencing multi-organ failure and death. Half got no nutrition for 3 days (unless requested). What happened?
After 6 months of follow-up, there was no statistical difference in the composite primary outcome of death-or-major-infection (infected necrotic pancreas, bacteremia, or pneumonia): 30% in the early-fed group vs. 27% in the late-fed group.
11% of the early-fed patients died, compared to 7% of the late-fed patients (non-significant statistically).
~62% developed necrotizing pancreatitis in each group.
Almost 70% of the patients assigned to the delayed strategy recovered to be able to eat, and did not require tube feeding.
This moderate-sized randomized trial won't change the perceived standard of care, which remains early enteral nutrition in patients with severe acute pancreatitis. It also illustrates the overlap and gray area in differentiating "ordinary" acute pancreatitis (who are advised to get no nutrition) from "severe" (defined here, who are supposed to get early enteric tube feedings).
As the definitions of "early" and "enteral" remain imprecise, physicians have significant flexibility in the management of severe pancreatitis:
"Early?" The current study seems to be the only randomized trial testing the timing of two equivalent enteral nutrition strategies, and found no difference. Is early "today," or anytime within 3 days? No one really knows the answer.
"Enteral?" The idea that nasojejunal feedings are preferable to nasogastric feedings in acute pancreatitis may be unfounded, as follows.
Nasojejunal vs. Nasogastric Feedings in Severe Pancreatitis
Post-pyloric feeding tube placement (nasojejunal, past the ligament of Treitz and pancreatic ampulla) has been traditionally advocated to avoid stimulation of the pancreas. This practice seems to have arisen from Dr. Dogma's physiology class. Nasojejunal feeding does reduce pancreatic stimulation, but no deleterious effects have been confirmed in actual people with pancreatitis receiving pre-pyloric feedings. Studies of animals with induced pancreatitis failed to show any harmful effect of nasogastric feeding.
In humans, 3 small randomized trials (1, 2, 3), found no differences in outcomes among patients with severe acute pancreatitis randomized to either nasogastric or nasojejunal feedings. I found no evidence making the counterpoint (that nasojejunal feedings are superior to nasogastric).
European guidelines (ESPEN 2006) advise:
Tube feeding is possible in the majority of patients with [severe] acute pancreatitis, but may need to be supplemented by the parenteral route. If gastric feeding is not tolerated the jejunal route should be tried.
American gastroenterology society guidelines (2013) advise:
In severe acute pancreatitis, enteral nutrition is recommended to prevent infectious complications. Parenteral nutrition should be avoided, unless the enteral route is not available, not tolerated, or not meeting caloric requirements. Nasogastric delivery and nasojejunal delivery of enteral feeding appear comparable in efficacy and safety .
(What about the American nutrition society, ASPEN? They hide their guidelines behind a paywall, making U.S. users pay twice for them, as our tax dollars funded much of the research that created them. They are not included here.)
This study fits the trend of most recent literature on nutrition in severe and critical illness, following the theme that the enteral nutritional strategy used does not measurably influence outcomes. The weakly consistent signals across studies seem to be, try to use the gut whenever possible, and try to delay TPN or limit parenteral nutrition to a minimum.
Clinical Takeaway: This moderate-sized randomized trial showed no benefit of starting enteral nutrition within 24 hours in patients with severe acute pancreatitis, compared to providing no nutrition at all for 3 days. Nasogastric feeding tube placement is appropriate for most patients with severe pancreatitis, according to professional societies' guidelines.
Olaf Bakker et al. Early versus On-Demand Nasoenteric Tube Feeding in Acute Pancreatitis. N Engl J Med 2014; 371:1983-1993.
European society nutrition guidelines (ESPEN)
American College of Gastroenterology guidelines
Nutrition in Acute Pancreatitis: Moving Full Circle or Moving Forward? (AGA website)
Definition of severe acute pancreatitis, by 2012 international consensus.


