Pleural catheters equal to pleurodesis for dyspnea relief from malignant effusions (TIME2)
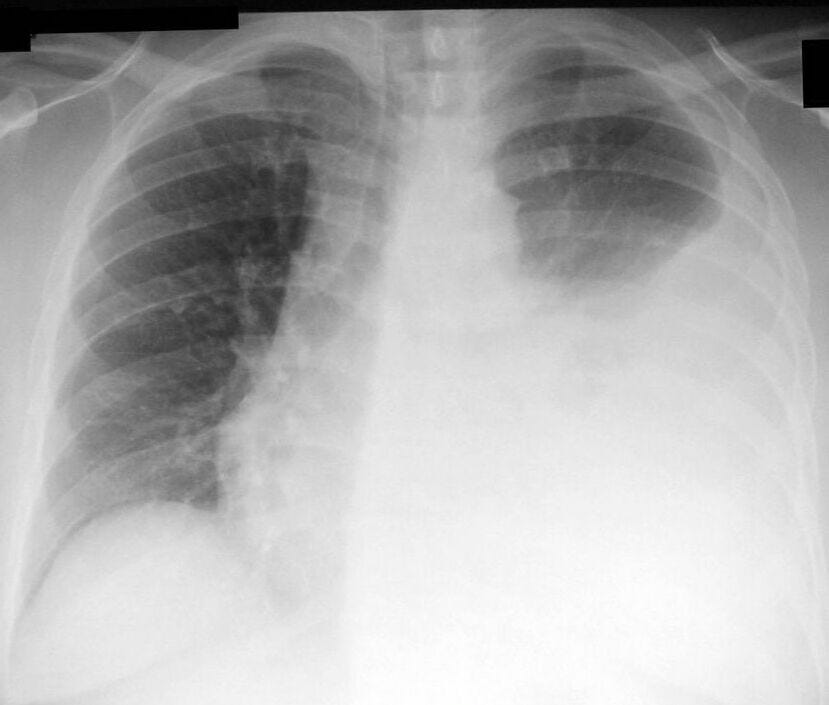
(image: Wikipedia)
In the TIME2 randomized trial published in the June 13 2012 JAMA, indwelling pleural catheters and talc pleurodesis were equivalent at reducing dyspnea over the 6 weeks following the procedure among 106 patients with malignant pleural effusions. Most patients receiving pleural catheters required no hospital stays, and overall had fewer repeat procedures than those receiving talc pleurodesis. After 6 months, patients with indwelling pleural catheters had slightly less dyspnea than those who had undergone pleurodesis.
However, patients receiving pleural catheters experienced more adverse events, including a few pleural infections. The trial was small, and given the near-equipoise in outcomes here, patient preferences should guide the choice of therapy for malignant pleural effusion.
Pleural catheters Vs. Talc Pleurodesis for Malignant Pleural Effusions
The development of a malignant pleural effusion after a cancer diagnosis is a sad and ominous sign: patients with malignant pleural effusions only live an average of about 4 months. Whether or not additional chemotherapy is pursued, an immediate emphasis must be made toward symptom relief, making the person's remaining life less uncomfortable and -- as much as possible -- free from the disabling and frightening symptom of dyspnea.
Existing guidelines recommend talc pleurodesis (instilled through a chest tube) as the first-line therapy. However, this requires hospitalization (on average, a week's stay), and malignant pleural effusions recur after talc pleurodesis about 30% of the time.
Given these limitations of talc pleurodesis, interventional pulmonologists and chest surgeons have increasingly adopted indwelling pleural catheters (like the PleurX catheter) as an alternative treatment for malignant pleural effusions. Indwelling pleural catheters have the advantage of outpatient insertion, but the disadvantage of ongoing violation of the body, and the requirement for home care & maintenance by the patient and her family.
Data to recommend either talc pleurodesis or indwelling pleural catheters over the other on efficacy or safety had been lacking.
What They Did
Helen Davies, Eleanor Mishra, Najib Rahman et al randomized 106 patients with malignant pleural effusion from 7 hospitals in the U.K. to undergo either talc pleurodesis through a chest tube, or placement of an indwelling pleural catheter. The trial was randomized but unblinded. Patients described their dyspnea daily for 6 weeks using a visual analog scale (= primary endpoint).
About half the patients in each group had either breast or lung cancer; 21 in each group were categorized as having "other" metastatic cancers.
What They Found
Dyspnea improved equally in both groups, with an improvement of ~24.5 points in the 100-point visual analog scale over the 6-week follow-up period. More than 75% of the patients in each group experienced a clinically significant improvement in dyspnea.
At 6 months, among the 43 surviving & available patients, those with indwelling pleural catheters described slightly less dyspnea than those receiving talc pleurodesis (about 12 points difference, statistically significant).
There was no difference observed in quality of life.
Hospital stays were shorter in the pleural catheter group: the vast majority did not require hospitalization, while most patients undergoing talc pleurodesis stayed in the hospital at least 4 days.
Need for Repeat Procedures: 12 of the patients undergoing pleurodesis required repeat procedures; only 3 of the indwelling pleural catheter patients did.
Adverse Events: Patients receiving pleural catheters had more adverse events than pleurodesed patients (40% vs. 13%). Most of these were nonserious (e.g., cellulitis, catheter blockage). However, an excess of 4 patients with pleural catheters had serious pleural infections (5 vs. 1, all occurring >50 days after catheter placement); one patient likely died from it.
Mortality: No firm conclusion could be drawn about any differences in mortality between groups.
What It Means
Pleural catheters and talc pleurodesis appear equivalent in relieving dyspnea in patients with malignant pleural effusions. (Technically speaking, this was a superiority trial and underpowered to prove equivalence, but any difference in efficacy is likely to be small.) The mishmash of relative risks and benefits -- e.g., pleural catheters require no hospitalization, but more maintenance -- are such that one procedure can't be recommended over the other from this data. But the great news is, both work.
Even with this information, deciding between talc pleurodesis and an indwelling pleural catheter is still a tough choice for a patient to make, and for the physician to guide them through:
The pleural catheter will get you in and out of the hospital faster, with less discomfort up front, but more inconvenience and cosmetic concerns after you go home, and also a slightly higher chance of problems like infection later on ... The talc pleurodesis would be uncomfortable and keep you in the hospital a week, but then you might be "done," with no more maintenance ... although then again, 30% of the time the fluid comes back and you might need more procedures if that happens. But overall, both procedures tend to work equally well at relieving your shortness of breath.
Bewildering, but since individual outcomes are unpredictable, both procedures work, and this decision usually takes place grounded in palliative goals of care, for most patients there is no right or wrong choice.
Davies HE et al. Effect of an Indwelling Pleural Catheter vs Chest Tube and Talc Pleurodesis for Relieving Dyspnea in Patients With Malignant Pleural Effusion. JAMA 2012; 307:2383-2389.


