Resuscitation Fluids in Critical Illness (Review)

Resuscitation fluids may be the most common intervention in critical care, with more than 200 million liters of normal saline infused each year in the U.S. alone. However, there is scarce evidence to guide the best use of resuscitation fluids in the ICU. John Myburgh and Michael Mythen’s review article in the September 26 2013 New England Journal of Medicine is a good place to start. Their most important takeaway is that resuscitation fluids can have harmful effects. Therefore, intensivists should “consider the use of resuscitation fluids as they would any other intravenous drug” — in other words, stop and think a bit more before using them.
Resuscitation Fluids in the ICU: Pearls
There is no such thing as an ideal resuscitation fluid; they each have flaws, and none has been demonstrated superior to the others in effectiveness or safety (with the possible negative exception of HES, below).
Any resuscitation fluid can contribute to interstitial edema, which may be have detrimental effects on ventilator weaning, cardiovascular function, wound healing, or other outcomes.
Although colloids have been believed to have superior “volume-expanding” effects over crystalloids, any advantage of colloids in hemodynamic response appears to be minimal in practice.
Normal saline given in large quantities can cause a hyperchloremic metabolic acidosis, and has been associated with renal injury.
Hydroxyethyl starches (HES) have harmful effects in many critically ill patients, and there seems to be little justification for their continued use, or for other semisynthetic colloid solutions.
Albumin appears safe and may be helpful in early sepsis, but has no definite advantages, and is too expensive to recommend as a standard resuscitation fluid.
Hypertonic saline (used to avoid producing edema) has not yet been proven safe.
Thanks for the Memories, Starling: Glycocalyx Ascendant
Remember the Starling principle you memorized in med school? The balance of hydrostatic and oncotic forces determines intravascular volume, vascular permeability, interstitial fluid resorption, etc.?
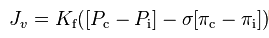
Proposed in 1897 and refined in 1932, it seemed useful for a while, but like many theories formed without the benefit of electron microscopes, Starling's missed the mark a bit. Turns out there’s something called the glycocalyx - a sugary glycoprotein matrix lining the capillary endothelium — which largely determines colloid oncotic pressure and vascular permeability. Read more on the glycocalyx. For its part, interstitial fluid is resorbed into the lymph system (not venules) under sympathetic nervous control.
Saline is Not Normal (But It Is Cheap and Effective)
Saline's designation as "normal" was based on an erroneous calculation of the salt concentration in blood as 0.9% back in 1882 (it's actually 0.6%). Saline is nearly isotonic with extracellular fluid, but frequently causes a hyperchloremic metabolic acidosis; the excess chloride has been blamed for immune and renal dysfunction. It's also a common reason for hypernatremia in hospitalized patients. However, saline is cheap, about $1.50 to $2 a liter, and is an effective resuscitation fluid; it's by far the most widely used globally. Hypertonic saline (3-7.5%) is sometimes used to maximize volume expansion while avoiding edema (such as in brain injured patients), but this has not yet been shown to be beneficial.
"Balanced" Salt Solutions as Resuscitation Fluids
So-called balanced salt solutions (Hartmann's and Ringer's solutions, a.k.a. lactated Ringer's) were designed to more closely approximate the composition of extracellular fluid by including potassium, calcium, and lactate or acetate as a more stable substitute for bicarbonate. More recently, a proprietary solution called Plasma-Lyte has been marketed a more physiologic balanced salt solution. None of these solutions exactly replicate the composition of extracellular fluid, and excess administration can cause hyperlactatemia and metabolic alkalosis. Lactated Ringer can cause hyponatremia and hypoosmolarity. Acetate-containing solutions can be cardiotoxic at high doses. If calcium is included and citrate-containing red cell transfusions are also given, microthrombi can result. No randomized trial has yet demonstrated the benefit of balanced salt solutions over ordinary saline (or vice versa). However, in a prospective observational trial, rates of renal failure fell after physicians were required to use balanced salt solutions instead of saline in one ICU.
Resuscitation Fluids: What's Inside
Albumin (4%) Saline (0.9% NaCl) Lactated Ringer's Plasma-Lyte Sodium (Na) 148 mmol/L 154 mmol/L 130 mmol/L 140 mmol/L Chloride (Cl) 128 mmol/L 154 mmol/L 109 mmol/L 98 mmol/L Potassium (K) none none 4 mmol/L 5 mmol/L Calcium (Ca) none none 1.5 mmol/L none Magnesium (Mg) none none none 3 mmol/L Lactate none none 28 meq (28 mmol/L) none Acetate none none none 27 mmol/L Gluconate none none none 23 mmol/L Tonicity 250 mOsml/L 308 mOsm/L 280 mOsm/L Isotonic (294 mOsm/L) Cost (est.) $125/dose $2 / liter $4 / liter $12 / liter
Albumin as a Resuscitation Fluid
Albumin (4-5% in saline) has purported hemodynamic advantages over crystalloid solutions as a volume-expanding resuscitation fluid. Physiologic studies have suggested a 1:3 ratio of albumin to crystalloid to achieve the same intravascular volume. In actual use (the SAFE study enrolling 7,000 ICU patients), the observed ratio was only 1:1.4, and patients in the albumin arm did not have any measurable advantage in hemodynamics (other than a slight improvement in central venous pressure). The colloid and crystalloid arms had identical rates of death and new organ failure. Post hoc analyses of SAFE showed:
An increased rate of death (RR 1.6) after 2 years for patients with traumatic brain injury.
A reduction in 28-day mortality in patients with severe sepsis (odds ratio 0.7).
Some consider albumin a wise choice as a resuscitation fluid for patients considered to be more at risk for volume overload (e.g., congestive heart failure, liver failure, or end-stage-renal disease). Others cite the SAFE subgroup analysis as an argument to use albumin in early sepsis. Given its narrow margin of benefit, at ~$100 a dose (compared to ~$2 for saline), albumin is too expensive to be recommended as a standard resuscitation fluid.
Hydroxyethyl Starches: Dangerous at Any Size?
Hydroxyethyl starches (HES) are made by modifying starch (polymeric glucose) molecules from potatoes or other plants, to make them resistant to enyzmatic degradation. This makes them stay in the circulation longer, increasing oncotic pressure. However, it also seems to cause organ damage in some patients as these molecules deposit in the kidneys, liver, and other tissues. Hydroxyethyl starches have been associated with increased death and renal failure in patients with severe sepsis, and regulatory authorities have advised against HES use in these patients. HES continues to be used as a resuscitation fluid in military trauma, major surgery, and in critically ill patients for its perceived superiority as a volume expander. However, like albumin, its theoretical 1 : 5 effectiveness ratio over crystalloid appears to be more like 1 : 1.3 in clinical practice. As these authors put it, given the potential risks, “the use of semisynthetic colloids for fluid resuscitation in critically ill patients is difficult to justify.”
Resuscitation Fluids: Take Home Points
These authors also advise us:
Use resuscitation fluids like any other intravenous drug: carefully and only in the doses necessary in appropriate clinical situations. Overuse of resuscitation and maintenance fluids result in interstitial edema, which might be harmful when excessive. Consider patients’ cumulative fluid balance and daily weights in the decision.
Temporary oliguria is expected after hypovolemia. Don’t use oliguria alone as a reason to give resuscitation fluids, especially if significant doses have already been given.
Think before giving any fluid challenges >24 hours after adequate resuscitation has been performed; the patient is usually not volume depleted.
Think before continuing hypotonic maintenance fluids after correcting a patient’s dehydration (e.g., hypernatremia, volume depletion); this may contribute to interstitial edema.
Consider starting norepinephrine early during resuscitation for patients with shock.
Saline is well-suited for patients with hypovolemia and alkalosis.
Albumin seems reasonable as resuscitation during early severe sepsis (but so does crystalloid).
Don’t give albumin to patients with traumatic brain injury.
Drs. Myburgh and Mythen are gentle proponents of using balanced salt solutions as first-line resuscitation fluids, suggesting: “Isotonic, balanced salt solutions are a pragmatic initial resuscitation fluid for the majority of acutely ill patients.” Their underlying argument seems to be, we should use the more expensive balanced salt solutions, but more cautiously than at present, which could blunt the increase in cost. Given the enormous volumes of resuscitation fluids infused each year around the world, they also rightly call for a large randomized trial to establish any relative benefit of one resuscitation fluid over another. John A. Myburgh and Michael G. Mythen. Resuscitation Fluids. N Engl J Med 2013;369:1243-51. DOI: 10.1056/NEJMra1208627 Normal saline causes renal failure? PulmCCM review.


