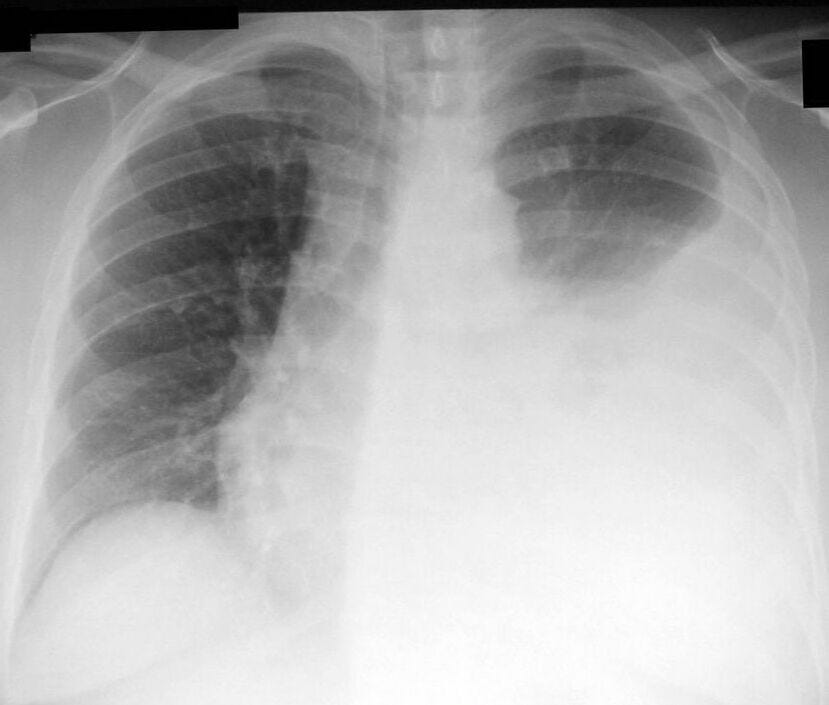
Should pleurodesis or PleurX drain be 1st-line Rx for malignant pleural effusion?
(image: Wikipedia)
There are an estimated 200,000 pleural effusions due to malignancy each year in the U.S. alone, and these represent an important cause of suffering and limitation in functional ability for people living with advanced cancer. Pleurodesis (using talc or other sclerosants) and placement of indwelling pleural catheters are both accepted, reasonable approaches to the management of malignant pleural effusions. In a recent JAMA article testing the two treatments for malignant pleural effusion, both appeared to be equally efficacious at relieving dyspnea.
So which should we recommend as first-line therapy for malignant pleural effusions? And if talc pleurodesis is chosen, is a more-invasive thoracoscopic technique superior to simple chest tube placement followed by talc slurry?
I was hoping for some sparks between Pyng Lee and Richard Light as they took opposite sides in the debate over whether pleurodesis or indwelling pleural catheters should be considered the preferred intervention, but none flew in the July 2012 Chest. Dr. Lee advises that thoracoscopic talc pleurodesis is preferable; Light argues an indwelling pleural drain is the best first-line therapy for malignant pleural effusion. In this situation of likely equipoise, the decision should be made on an case-by-case basis, taking into account patient preferences, local expertise and some of the finer points that have emerged from recent studies:
In the 2012 JAMA TIME2 randomized trial of 143 patients with pleural effusions from various malignanices (lung cancer, breast cancer, etc), pleurodesis by chest tube with talc slurry (not thoracoscopic talc poudrage) appeared equally effective as indwelling pleural catheter placement at relieving dyspnea.
Indwelling pleural drain placement requires no hospital stay for most patients (it's an outpatient procedure), while talc pleurodesis requires a hospital stay of several days, on average.
Talc pleurodesis requires repeat pleurodesis for a recurrent malignant pleural effusion as often as 30% of the time (22% in the TIME2 trial). Patients undergoing indwelling pleural drain placement don't usually need additional procedures, although many need extra attention for minor catheter blockages, for example.
However, once someone has a successful talc pleurodesis, they're done, and don't have to walk around with a drain and the cosmesis / body image concerns that go with it. (That said, as many as 45% of patients with indwelling pleural drains achieve pleurodesis too, at which point the catheter can be removed.)
Talc is the most often used agent but hasn't been tested against other sclerosants (tetracyclines, etc.), which are also reasonable options.
Large-particle talc should be used if talc pleurodesis is elected. There are reports of ARDS associated with small-particle talc, but none in a multicenter series of >580 patients receiving large-particle talc pleurodesis.
Serious complications of indwelling pleural drains were rare in TIME2 and in a pooled analysis of 19 studies (n=1370) by Van Meter (J Gen Intern Med 2011); the incidence of empyema after indwelling pleural catheter placement is probably about 3%.
It's unclear whether thoracoscopic talc poudrage (inducing a pneumothorax on the affected side, invading the thorax with a pleuroscope, and spraying aerosolized talc) is at all superior to the simpler procedure of talc slurry through a standard chest tube. The Phase III intergroup study showed a benefit in breast and lung cancer-related effusions; Dr. Lee argues that signal is real, while Dr. Light questions it as an inappropriate post-hoc over-reading of the data counterbalanced by harms in the other patient subsets. Thoracoscopic talc poudrage is a significantly more invasive procedure, requiring specialized expertise (an interventional pulmonologist or chest surgeon) and often general anesthesia.
Lee P. Point: Should Thoracoscopic Talc Pleurodesis Be the First Choice Management for Malignant Effusion? Yes. Chest 2012;142:15-17.
Light RW. Counterpoint: Should Thoracoscopic Talc Pleurodesis Be the First Choice Management for Malignant Pleural Effusion? No. Chest 2012;142(1):17-19.


