That Fallible IVC
Jon-Emile S. Kenny [@heart_lung]
A 58 year old man with ethanol-related cirrhosis is admitted to the floor with anuria and a rising creatinine. Over the day, serial ultrasounds of his inferior vena cava [IVC] consistently reveal that it is diminutive and collapsing. He receives many liters of crystalloid without much change in his urine output. In the middle of the night, a rapid-response is called for dyspnea and desaturation with a lung ultrasound revealing bilateral and ubiquitous B-lines; he is placed on non-invasive positive pressure ventilation and given IV furosemide, but his blood pressure continues to fall. Repeat ultrasonographic assessment of his IVC reveals, again, a small and collapsible great vein; the overnight resident reaches for another liter of normal saline.
Another recent publication has analyzed the diagnostic accuracy of using IVC assessment for detecting fluid responsiveness in the ‘spontaneously breathing’ patient. Importantly, in this study, it is clear that no patients are receiving any form of invasive or non-invasive ventilation. This is notable, as a patient may breathe ‘spontaneously’ while triggering invasive [e.g. pressure support] or non-invasive [e.g. BiPAP] forms of respiratory support. What was ultimately found was that an IVC collapsing index more than 42% revealed an excellent specificity, but a fairly poor sensitivity for the prediction of fluid responsiveness. These findings are important and somewhat similar to another, previous study which considered a similar patient population, although it is unclear if this earlier study excluded spontaneously breathing patients receiving assisted ventilation.
Specificity
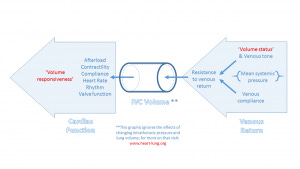
Specificity is a measure of false positives. Within this context, a false positive would be a patient with a collapsing IVC [therefore deemed to be a fluid responder] who ends up being resistant to fluid. The collapse of the IVC occurs under the influence of four, independent variables: 1. The inspiratory fall in intra-thoracic pressure 2. The inspiratory rise in intra-abdominal pressure 3. The inspiratory change in cardiac function and venous return which together determine the pressure within the IVC and 4. The method of patient breathing [e.g. diaphragmatic versus thoracic]. Therefore, understanding what would cause an IVC to collapse in a fluid non-responder requires a refresher in Guytonian physiology, upon which I have previously commented extensively. In summary, an IVC will ‘inappropriately’ collapse in a fluid resistant patient when 1. The patient is inspiring excessively, 2. The intra-abdominal pressure is abnormally high [e.g. ascites, intra-abdominal hypertension] and 3. When the venous return curve intersects the plateau of the cardiac function curve at a relatively low intra-luminal [i.e. within the vessel] pressure. This latter situation will occur when both venous return to the heart is low and cardiac function is relatively impaired; for example, a patient with very poor venous tone [e.g. cirrhosis, sepsis, adrenal insufficiency, venodilating medications] and poor cardiac function [e.g. from alcohol-related cardiomyopathy]. Consider the diagram below which depicts the determinants of the pressure within the IVC, prior to an inspiration.
Another exceptionally important, and often ignored, determinant is how positive intra-thoracic pressure [whether applied invasively, non-invasively, or develops pathologically – e.g. auto-PEEP], also alters venous return. Positive pressure facilitates collapse of the IVC; this has been known for many decades! Pressurization of the upper abdomen by the application of end-expiratory pressure will make the IVC collapse much more readily when the patient triggers a breath. In healthy volunteers, this has been demonstrated. Consequently, the aforementioned could result in a ‘false positive’ IVC collapse in a fluid non-responder and impair specificity. Importantly, in the study at hand, no patients were receiving ventilation of any sort and this may account for its excellent specificity [i.e. few false positives].
Sensitivity
Sensitivity is a measure of false negatives. Within this context, a false negative is a patient with a relatively engorged, unwavering IVC who will still respond to an IV fluid challenge. In the study under question, like its predecessor, sensitivity tended to be quite poor, that is, many patients with plump IVCs can still respond to fluid. Why might this be so? Considering the analysis above, many factors may play a roll. For example: if the patient does not inspire greatly or if the patient uses thoracic wall muscles rather than the diaphragm; if the rise in intra-abdominal pressure is poor or if the venous return curve intersects the ascending portion of the cardiac function curve at a relatively high intra-luminal pressure. This latter situation may occur in patients with both good venous return and preserved cardiac function. When a patient has normal venous tone and is relatively hypervolemic, the abdominal venous beds have been described as being like ‘West Zone III’ within the lungs. Decent of the diaphragm in this situation maintains or augments venous return through the great vein which would maintain its volume and size. If this occurs in a patient with good cardiac function, the venous return curve may still intersect the ascending portion of the Frank-Starling curve, and the patient will be volume responsive.
Volume status versus volume responsiveness
On this final point, it should be apparent that a patient’s ‘volume status’ [i.e. the degree of plasma volume] is physiologically distinct from a patient's ‘volume responsiveness’ [i.e. whether or not an increase in plasma volume will result in an increase in cardiac output]. As in the diagram above, volume status is but one determinant of venous return to the heart; however it is how the heart handles its venous return that defines volume responsiveness. It follows that a patient can be hypervolemic and volume responsive or hypovolemic and volume unresponsive. For further information please watch these physiology lectures [Chapters 6D, 8A & 8F]
Bedside ultrasound is a great power; it therefore demands great responsibility,


