The Latest in Critical Care: August 13, 2025
Altshock-2, Midlines vs. PICCs, Whether to interrupt feeding before extubation
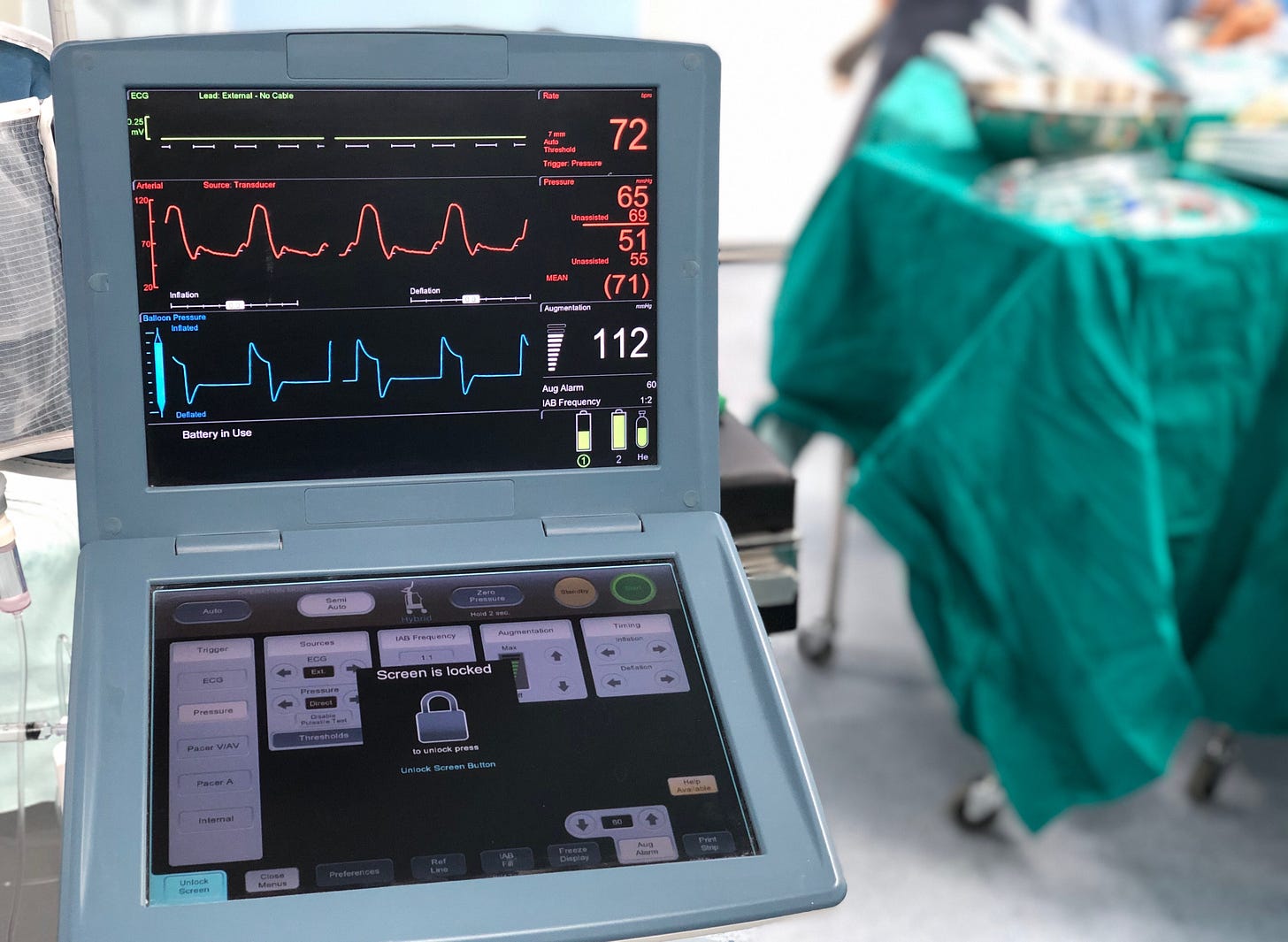
Intra-aortic balloon pumps for cardiogenic shock from heart failure (Altshock 2)
Intra-aortic balloon pumps were once the care standard for cardiogenic shock due to myocardial infarction, despite the absence of evidence of benefit. It always seemed better to do something more than nothing.
The Impella™ device supplanted IABP for cardiogenic shock from acute STEMI, after demonstrating benefits in selected patients despite a high rate of complications.
IABP continued to have a perceived role as salvage support therapy for patients with cardiogenic shock due to congestive heart failure, who are awaiting left ventricular assist device placement or heart transplant.
Among 101 patients with decompensated CHF and cardiogenic shock at multiple centers in Italy, those randomized to early IABP had roughly the same rate of survival/successful bridging therapy as usual care (81% vs. 75%). The trial was stopped early for futility because enrollment was slow and there was no statistical possibility of finding a benefit.
This failure appeared to have been easily predictable at the design phase, when they overestimated an implausible 20% absolute benefit with IABP (estimating the primary outcome would occur in 75% in the intervention arm and 55% in the controls), which conveniently produced a requirement of enrolling only 200 subjects by their initial (incorrect) power calculations.
Midline catheters malfunction far more often than PICCs
Midline catheters are more easily placed in an arm vein than peripherally inserted central catheters, and have become more widely used in recent years.
But they may not work as reliably as PICCs. In a trial randomizing 294 patients to midline or PICC, a third of midlines malfunctioned, compared to only 7% of PICCs. This usually represented partial occlusion of the catheter (27% vs. 5%).
Adverse events were uncommon in both groups but nominally higher in the midline arm (5.2% vs. 1.5%), and none appeared severe (e.g., thrombophlebitis, local infection, bleeding at insertion site) or reached significance.
Enrollment was lower than expected, and the trial was likely underpowered to confirm a difference or rule it out.
There were no bloodstream infections identified in either group.
Most commonly, malfunctioning midlines stop drawing blood but continue to be useful for infusions. PICCs are considered more likely than midlines to cause central vein stenosis, compromising future dialysis access.
—Bentridi et al, JAMA Network Open 2025 and editorial
Is interrupting enteral nutrition before extubation necessary?
Extubation is sometimes delayed to permit time for gastric emptying in patients receiving enteral nutrition, on the premise that this will reduce aspiration and reintubation risk. This is probably unhelpful.
Among 1,130 mechanically ventilated patients at 22 ICUs in France, those who were randomized to continued enteral nutrition until extubation had similar outcomes as those who underwent 6 hours of fasting and gastric suctioning before extubation:
Extubation failure (17% with continued tube feedings, 17.9% with fasting)
Pneumonia (1.6% vs. 2.5% with fasting)
However, assignments were unblinded, which could have impacted extubation decisions.
—Landais et al, Lancet Respiratory Medicine 2023