Theophylline as add-on therapy was no use in preventing COPD exacerbations
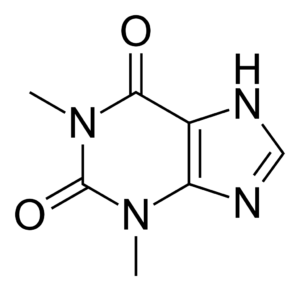
Theophylline is derived from methylxanthine, naturally present in tea and cocoa beans. Initially used medically in 1895 as a diuretic, theophylline was one of the first drugs for asthma and COPD/emphysema (beginning in 1922), after its bronchodilation effects were discovered. Theophylline also has cardiac and central nervous system stimulant side effects and can produce tachyarrhythmias and seizures. High theophylline doses are required for effective bronchodilation (plasma concentration of 10–20 mg/L) but these doses also increase the drug's side effect risks. Theophylline thus fell out of wide use after safer, more effective inhaler therapies were introduced for asthma and COPD. For COPD, the Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends theophylline only be used when inhaled bronchodilators are not an option (unavailable or unaffordable, mainly in the developing world). However, there has remained a cohort of theophylline true-believers -- patients who swear by the drug and refuse to stop taking it, and physicians who still believe its benefits outweigh its risks. When theophylline is used, it's often in the hope of preventing COPD exacerbations. A group of investigators in the U.K. explored whether lower-dose theophylline might improve outcomes in COPD, with acceptable adverse effects. About 1,500 patients with moderate-to-severe COPD with repeated exacerbations were randomized to either low-dose theophylline (200–400 mg daily to attain plasma concentration of 1–5 mg/L) or placebo for 12 months. All patients received inhaler therapies: 80% got triple therapy (inhaled steroids, long-acting β-agonist, and a long-acting antimuscarinic drug). After a year of follow-up, there was no difference in exacerbations (~1,700 in each group). Theophylline was fairly well tolerated, with no excess cardiac risks, and a mild increase in GI side effects, headaches, and nausea. Most physicians are not prescribing theophylline for COPD, and this study may further discourage its use. Azithromycin has been shown to reduce COPD exacerbations in severe COPD, but carries an FDA warning for risk of sudden cardiac death. Roflumilast (Daliresp) also reduces COPD exacerbations in patients with a chronic bronchitis phenotype with frequent exacerbations. Limited evidence suggests aspirin may help prevent COPD exacerbations.
Source: JAMA


