Thrombectomy vs. anticoagulation alone for intermediate-high risk PE (STORM-PE trial)
Removing clot quickly improves physiology, but where's the long-term data?
Patients with pulmonary embolism severe enough to cause hypotension (so-called massive PE) are at high risk for death and should receive systemic thrombolytic therapy and/or invasive interventions.
Those who have adequate blood pressure and no evidence of right heart failure should receive anticoagulation alone, because the risks of more aggressive interventions are believed to outweigh any potential benefits.
For patients in the middle, with right heart strain on imaging, elevated cardiac markers, or other high-risk features (but not overt hypotension or shock), the ideal management is unknown. Should they receive invasive interventions, lower-dose systemic thrombolytics, or anticoagulation alone?
The challenge from both a research and a practical clinical perspective lies in the heterogeneity of the intermediate-risk category, which can comprise patients ranging from a minimal echocardiographic abnormality and hypertension to those with impending shock.
Observed mortality ranges from ~3% to ~15% in this group, increasing in the so-called intermediate-high subgroup who have both troponin elevations and right heart strain, and with comorbidities (e.g., preexisting heart failure).
Patients with intermediate-risk PE commonly undergo catheter-directed thrombolysis or mechanical thrombectomy at advanced centers offering these treatments. Research has shown these interventions can improve echocardiographic or short-term clinical parameters, but have not yet shown improvements in mortality or other patient-centered outcomes compared to anticoagulation alone.
Catheter-directed thrombolysis brings risk of major bleeding (which has varied from almost none to 10% in clinical trials), while mechanical thrombectomy has procedural (and bleeding) risks.
Most trials have been funded by industry, sometimes involving large direct payments to individual investigators and to their institutions (which has become a standard practice in device trials), and designs tilted toward favorable findings.
A prime example was the PEERLESS trial, which concluded that mechanical thrombectomy (with Inari’s device) was superior to catheter-directed thrombolysis for intermediate-risk PE—but this was driven mainly by fewer ICU admissions, an easily gamed variable (as most patients are observed in the ICU after thrombolysis, but not necessarily after thrombectomy).
More fundamentally, no randomized trial had tested mechanical thrombectomy against anticoagulation alone. Although some centers have begun intervening on most intermediate-risk PEs, anticoagulation remains the ostensible care standard, provided in the majority of cases when invasive therapies are not available (such as the weekend at some advanced centers).
The central unanswered question, then, has been whether early thrombectomy or thrombolysis improves outcomes over anticoagulation (in excess of their risks), in which case they should be more commonly performed; or whether these invasive therapies should be reserved for patients who are deteriorating.
The STORM-PE Trial
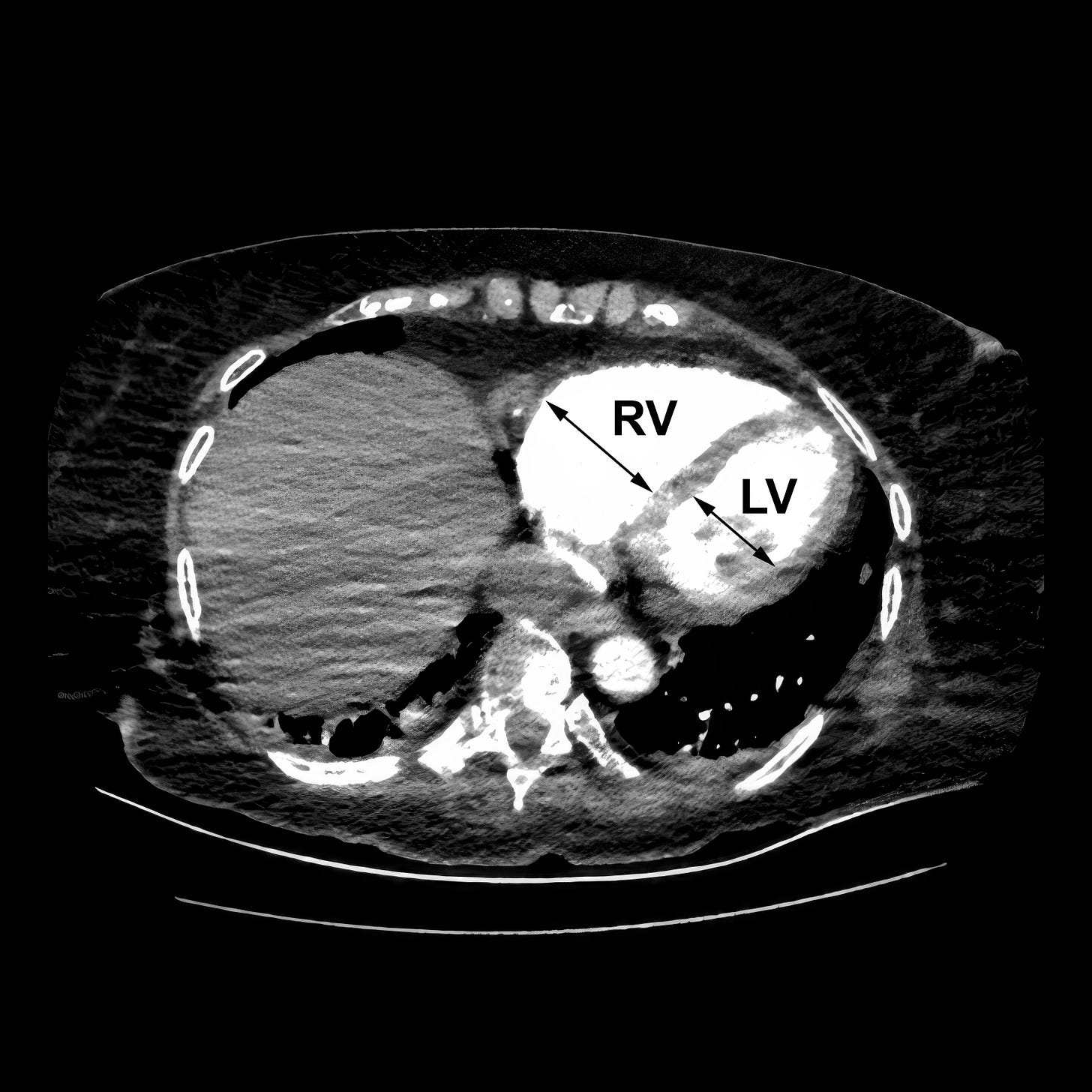
In STORM-PE, 100 patients at 22 centers in the U.S., Canada, New Zealand, and Poland with intermediate-high risk PE (defined as normotensive but with an elevated RV/LV ratio on CT and either elevated troponin or BNP, without active cancer) were randomized 1:1 to undergo mechanical thrombectomy with Penumbra’s Lightning Flash™ system plus anticoagulation, or anticoagulation alone.
During thrombectomy, mean pulmonary artery pressures dropped by 3 to 13 mm Hg in most patients.
Patients underwent repeat CT scans 48 hours later, which showed that the thrombectomy-treated patients had a greater reduction in RV/LV ratio (0.52±0.37 vs 0.24±0.40 in the AC arm, a difference of 0.27).
They also had improved physiologic parameters: a greater reduction in heart rate and in the NEWS2 score (a predictor of deterioration), and more patients were weaned off oxygen. All the patients treated with thrombectomy had resolution of tachycardia, compared to 57% of those treated with anticoagulation alone.
There were no major adverse events or bleeding attributed to thrombectomy.
Three patients in the anticoagulation arm (5.7%) required rescue therapies, vs. one (2.1%) in the thrombectomy arm. Two patients died of PE-related complications, both in the thrombectomy arm.
Penumbra funded the trial, and reported the following payments to the investigators between 2018 and 2024, according to the CMS Open Payments website. These were categorized as direct payments (e.g., for consulting or speakers’ fees), distinct from research funding, food and beverage, or travel and lodging.
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.