Thromboelastography (TEG/ROTEM™) for bleeding: Review (Part 2: Evidence for Use)
Does TEG actually help, and does it have a role in the MICU?
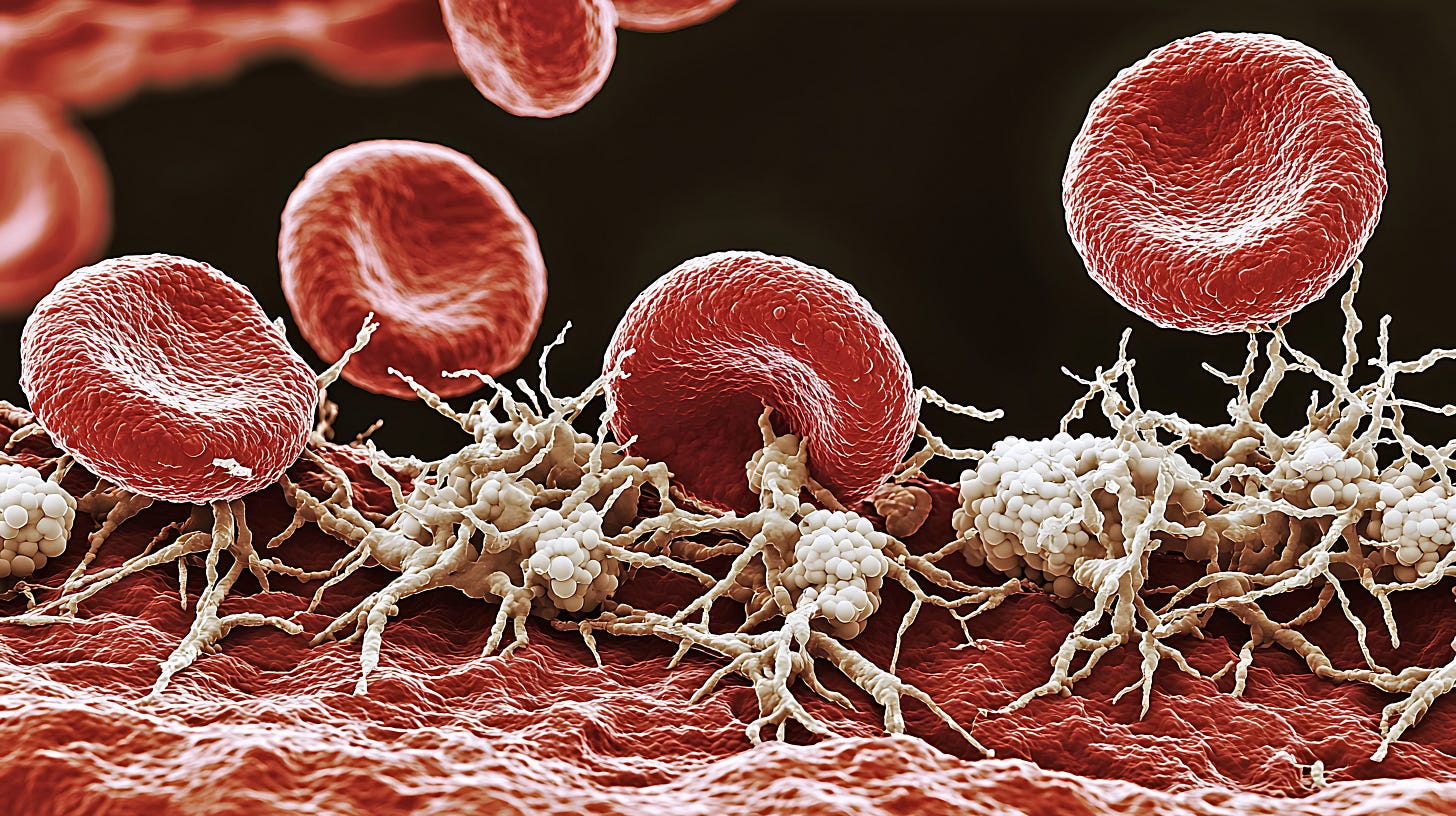
Viscoelastic testing, a.k.a., thromboelastography or rotational thromboelastometry (ROTEM™), is a method of analyzing clot kinetics and mechanical properties to better guide the management of severe hemorrhage.
Read part 1 of this review for a brief overview and video of the basic principles of the tests.
Invented in 1948, VET/TEG/ROTEM (called TEG for simplicity here) has been increasingly used by surgeons since the 1990s as point-of-care devices have become more accessible and user-friendly. TEG’s greatest uptake has been in trauma, cardiac surgery, and liver transplantation.
Evidence for Thromboelastography in Hemorrhage Management
Trauma patients, liver transplant recipients, and cardiac bypass patients are all at risk for disorders of fibrinolysis: too much (hyperfibrinolysis, leading to uncontrolled hemorrhage, treated with antifibrinolytic agents like tranexamic acid) or too little (fibrinolytic shutdown, leading to thrombosis, and treated supportively or with VTE prophylaxis).
TEG is a widely-used test to rapidly identify and differentiate these post-surgical fibrinolytic phenotypes.
Although TEG doesn’t pinpoint specific factor levels and only indirectly reflects platelet function unless adjunct assays are used, it can quickly guide transfusion of FFP (for slow clotting = a long R), cryoprecipitate or platelets (for poor clot kinetics = high K, or low clot strength = low maximum amplitude or MA) in bleeding surgical patients. TEG is usually performed in concert with conventional lab testing.
It can help identify post-operative bleeding: if a hemorrhaging patient’s TEG shows normal clotting, it may help drive the decision to re-explore surgically.
TEG has one undeniable advantage over conventional coagulation testing: it’s fast, with initial results available within 10 minutes or so. Its adoption may therefore have been inevitable in ultra-high-acuity surgical specialties. Viscoelastic testing point-of-care machines are common features in O.R.s in major surgical centers, eliminating laboratory turnaround times.
Randomized trials have shown that TEG can reduce the amount of blood products transfused, and possibly the need for invasive interventions to stop bleeding, but its effect on mortality (if any) remains inconclusive (see reviews by Cochrane, BJA). Trials have been mostly in cardiac surgery, highly heterogeneous and at high risk for bias. The TACS trial (Circulation 2016) was perhaps the largest and best-conducted.
The use of TEG has been endorsed in some surgical societies’ guidelines for management of hemorrhage (e.g., EAST, ASA, STS/SCA, and a European consensus document).
Does TEG have a role in the MICU?
Thromboelastography has had limited diffusion into non-surgical critical care settings to date. TEG may have a role in high-acuity patients who are bleeding or at risk for bleeding or who have difficult-to-interpret coagulation labs.
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.