Ventilator bundles (VAP bundles) not evidence-based, shouldn't be standard care
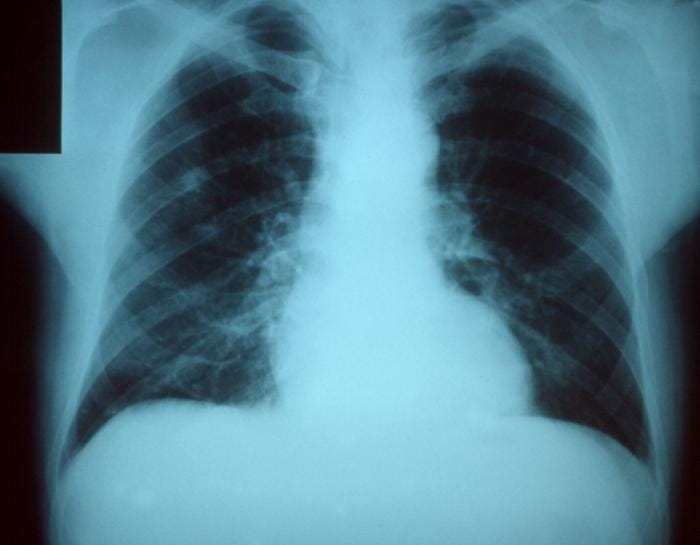
(image: Wikipedia)
Anyone who has ever rounded in an ICU with a nurse manager knows that challenging or questioning the utility of the ventilator associated pneumonia (VAP) bundle is a losing proposition -- one likely to get you labeled as a wiseguy troublemaker. Thanks to ventilator bundles' endorsement by the nonprofit Institute for Healthcare Improvement, and their consideration by policymakers as a pay for performance measure, hospital administrators have scrambled to implement ventilator bundles with almost the force of law. You might assume that all this effort is based on convincing evidence that VAP bundles improve outcomes and mechanically ventilated patients. But according to Naomi O'Grady, Patrick Murray, and Nancy Ames' grand rounds in the June 20th 2012 JAMA, you'd be mostly wrong. They deconstruct the IHI's “VAP bundle” (actually, they point out, it's a "ventilator adverse event prevention bundle," including measures unrelated to pneumonia prevention), and present the evidence for each element of the bundle, which skeptics will be unsurprised to hear, isn't so robust after all. In fact, they say:
No large randomized study has demonstrated that reducing VAP using any VAP prevention strategy, including those in the IHI bundle, is associated with improvements in clinical outcomes.
In case you don't have it tattooed on your forearm yet, here's a list of of what's inside the so-called ventilator bundle:
Elements of the IHI Ventilator Bundle ("VAP Bundle")
Elevation of the head of the bed to 45°
Daily sedation vacation and assessment of readiness to extubate
Daily oral chlorhexidine rinses
Proton pump inhibitors or H2 receptor antagonists
Anticoagulants or compression devices
Elevating the head of the bed appears to be helpful. Two small studies show that a 45° elevation reduce the incidence of VAP dramatically. However, this type causes sedated patients' heads to slump over; but the best-conducted study showed that 45° is rarely attained, and that 30° or even as little as 10° (which appears to have become standard practice) is likely just as beneficial. Daily sedation interruptions are known to reduce the duration of mechanical ventilation, especially when coupled with daily spontaneous breathing trials. While it is inferred that this would also decrease the risk for ventilator associated pneumonia, no study has ever shown this. Authors worry that in surgical or trauma patients, regular scheduled interruptions of continuous analgesia might be detrimental. Chlorhexidine mouth rinses have been associated with a lower incidence of VAP in cardiac surgery and trauma patients, but several studies have failed to replicate this finding in other patient populations, including the much larger general MICU population in which they are more commonly used [Labeau Lancet ID ... Chlebicki Crit Care Med]. Authors criticize the 3 often cited studies [1, 2, 3] that observed the benefit from implementation of the of the VAP bundle, pointing out that 2 of these studies did not report adherence rates with the bundle, and all 3 were subject to the time effect and/or Hawthorne effect inherent to these types of clinical trials: overall care or unmeasured aspects of care may improve during any quality improvement initiative, due to cultural factors, motivation of staff, etc. -- especially when participants know they are being observed. They also highlight several interventions that may show more promise than the supposedly-awesome VAP bundle elements:
Lateral, head-down (rather than supine) positioning reduced VAP in infants, and a randomized trial in adults is underway.
Subglottic suctioning with a continuously-sucking device reduced VAP incidence in several studies.
Silver-coated endotracheal tubes can also reduce VAP incidence. These cost $100, rather than a few bucks for a standard ET tube.
The as-disgusting-as-it-sounds "mucus shaver" can periodically clean the endotracheal tube of biofilm-forming secretions, potentially reducing the incidence of VAP.
The technological advances in endotracheal tubes that may reduce the risk of VAP were also reviewed by Fernandez et al in Chest 2012.
This is at heart an anti-guideline, anti-quality improvement editorial that implicitly questions the legitimacy of quasi-official institutions to impose mandates that would override individualized decision-making by physicians. A lot of things we do don't have great evidence behind them; we do them because they might help, or seem likely to help with a minimum of cost or risk. The evidence of benefit for some of the alternative VAP-reducing interventions mentioned is just as scant, and their cost may be much higher, if implemented widely. Physicians rightly bristle at being forced to do things by guidelines when evidence isn't supportive. Another editorial in Critical Care Medicine in January by Neil Halpern, Kaye Hale, Kent Sepkowitz and Stephen Pastores blasted the whole VAP-hunting exercise on these grounds, quoting management guru Peter Drucker: "There is nothing so useless as doing efficiently that which should not be done at all." I have to note that nowhere here do the authors quantify the downsides of our widespread implementation of the ventilator bundle. Even if our widespread faith in it is misplaced, so what? It's true that like virtually all other measures that have been proposed as candidates for pay for performance measures, there is little justification for such use of the ventilator bundle. But -- assuming no one is threatened with a cut in their paycheck or insurer payments for less than full compliance -- what's the big deal with a little well-intentioned mouthwash and bed repositioning (and mucus shaving, if you're into that)? O'Grady NP et al. Preventing Ventilator-Associated Pneumonia. Does the Evidence Support the Practice? JAMA 2012;307:2534-2439.


