Bicarb for AKI + acidosis prevents dialysis needs in the ICU (BICARICU-2 trial)
High-concentration NaHCO3 seemed to help in underpowered trial
Correction to our last correction: Thanks to Dr. Thomas Zeuner for informing us that norepinephrine dosing is not reported in tartrate units “commonly in Europe”; this may be a convention that is unique to France. Come on, France!
In this chart on neuroprognostication, it should have been “neuron-specific enolase <17 µg/L”, not “>”. These errors are regretted and corrected; now, on to the show.
Critically ill patients with acute kidney injury commonly become severely acidemic, which (at pH ≤ 7.1-7.2) is associated with impaired cardiac contractility, reduced effectiveness of vasopressors, and increased risk for cardiac arrhythmias.
But is the acidemia or the underlying illness (e.g., sepsis with lactic acidosis) causing these physiologic derangements? For example, by contrast, DKA patients commonly tolerate pH <7.0 without cardiac dysfunction.
In hypoperfusion-induced lactic acidosis, the argument goes, giving bicarbonate can be counterproductive by:
increasing intracellular acidity while making the arterial pH look (uselessly) better;
infusing a high sodium load (for NaHCO3), worsening volume overload, causing pulmonary edema and respiratory failure;
reducing ionized calcium levels, when calcium binds to albumin at increasing pH
For hyperchloremic acidosis, in which actual bicarbonate losses commonly occur (e.g., diarrhea, renal tubular acidosis), the rationale for bicarbonate therapy is stronger.
There is no strong consensus as to whether or when to provide bicarbonate for severe acidemia; sepsis guidelines have suggested pH <7.2 as a threshold, if significant AKI is present.
The BICARICU-1 trial (Lancet 2018) found that among 389 patients at 26 French ICUs with pH < 7.2 with normal pCO2, those randomized to sodium bicarbonate infusion did not have improved outcomes over usual care. The prespecified subgroup with the most severe AKI, though, had lower mortality and need for dialysis when treated with bicarbonate infusions.
A larger trial was therefore performed.
The BICARICU-2 Trial
At 43 adult ICUs in France between 2019 and 2023, 640 patients with AKI and severe acidemia (pH < 7.20) were enrolled.
They were sick: over half had septic shock, 75% were vented, and >80% were on vasopressors, with a median creatinine of ~2.2 at enrollment and pH of 7.15 with serum bicarb of 12-13 mEq/L.
Patients were randomized to either sodium bicarbonate infusion (4.2%, targeting pH≥7.30, 125-250 mL bolus followed by up to 1,000 mL total in 24 hours, pH followed with frequent ABGs) or usual care.
The protocol recommended but did not mandate when to start dialysis in either group.
Results
There was no difference in mortality at 90 days (62.1% vs. 61.7%).
That said, the confidence interval spanned a 7% reduction to an 8% increase in mortality, because in the design, the investigators hypothesized that bicarb would produce a 10% absolute mortality reduction from an 80% mortality in the control arm. This kind of wishful thinking keeps the enrollment numbers down and makes the trial more financially feasible, at the expense of certainty.
This meant that the trial was going to almost certainly be statistically neutral no matter the findings; we got lucky that the numeric mortality was equal in both arms.
Notably, patients who received sodium bicarbonate had a much lower rate of renal replacement therapy (35% vs 50%, significant) in the intention-to-treat analysis.
In the per-protocol or “as-treated” analysis, which breaks randomization to consider patients according to the treatment they received, the difference in need for RRT was smaller (38% vs 47%) but still significant. (Forty-seven control patients, or 15%, crossed over to receive bicarbonate.)
Patients randomized to bicarbonate therapy who required dialysis/CRRT were able to delay its initiation longer.
There were therefore fewer vascular catheters placed in the bicarbonate arm, which dwelled for shorter periods, and those patients had fewer recorded bloodstream infections (4% vs 9%).
The reduced need for RRT occurred despite the bicarbonate arm patients receiving about 1L more in fluid over the first 24 hours, compared to controls.
There was no clear increase in need for mechanical ventilation in the bicarbonate-treated arm.
Because investigators and care teams knew the treatment assignments, it’s impossible to rule out unmeasured treatment differences between groups. For example, dialysis could have been started systematically earlier (without conscious intent to bias the results) in control patients who were “on the fence” for needing RRT.
Discussion
Sodium bicarbonate infusions (for severe acidemia with AKI mostly due to septic shock) did not reduce mortality in this underpowered trial, but did reduce the use of renal replacement therapy.
Because dialysis initiation is a subjective decision, it’s particularly subject to bias. That said, the consistent signal of reduced RRT need across BICARICU-1 and 2 is interesting.
Most clinicians in the U.S. were already infusing bicarbonate for patients with metabolic acidosis and a pH < 7.15.
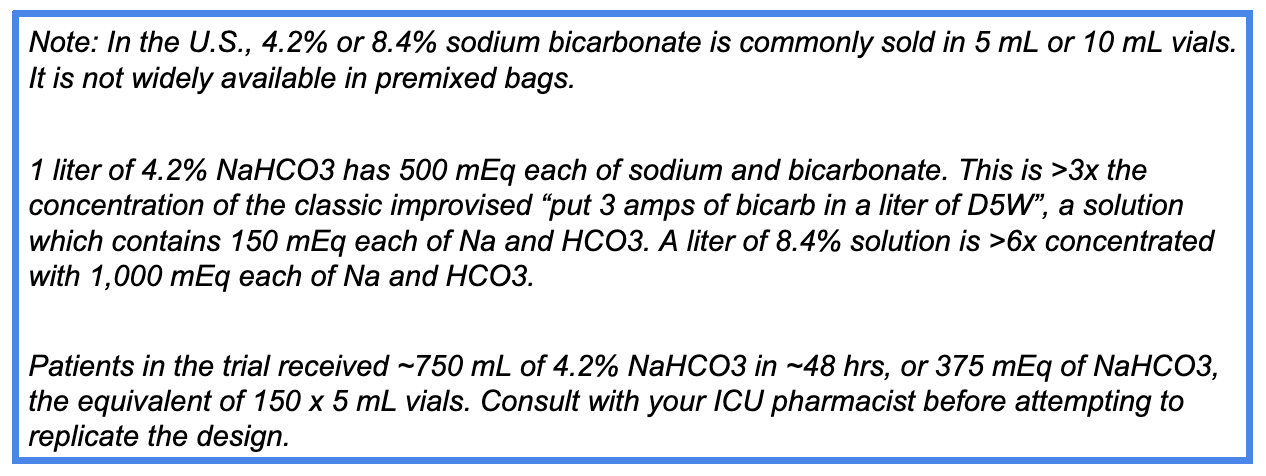
Replicating the trial design would require consultation with your ICU PharmD, as infusable 4.2% NaHCO3 solutions may require local mixing/compounding.
With its lack of apparent adverse events and suggestion of benefit in reduced need for RRT, the BICARICU-2 trial provides “good enough” reasons to enhance the practice of infusing sodium bicarbonate for patients with severe acidemia and AKI. In practical terms, this would mean using more concentrated NaHCO3 solutions, more consistently.




I think it is one of the most important studies of the year.
Of course, the 90-day mortality endpoint is BS because acidosis and AKI would be treated anyway in both groups.
However, it was highly plausible that loading the patient with bicarbonate would delay or obviate dialysis, as long as the patient urinates.
My take is that you don’t need to replicate their bicarb dilution. It is a first-order and dose-dependent effect. Give as necessary.
It would be interesting to see if there was a difference based on the delta/delta value. I would expect patients with a higher contribution of the normal gap acidosis to have a greater benefit from the bicarb as this is coming primarily from the AKI. It may be that patients with a greater contribution of the lactic acidosis have worse outcomes.