Guideline review: Transfusing fresh frozen plasma and platelets in critical illness
Unknown risks and benefits lead to wide variation in practice
Coagulation abnormalities (e.g., an elevated international normalized ratio or INR) and thrombocytopenia are present in most severely ill patients.
Fresh frozen plasma and platelets are commonly transfused for patients perceived to be at high risk of bleeding or who are undergoing invasive procedures.
Transfusion practice patterns vary widely, and many transfusions of plasma and platelets are probably unnecessary. In a recent review, as many as 20-25% of plasma transfusions were performed prophylactically for patients who were not bleeding, not about to undergo invasive procedures, and had INRs <3.0. (Haeren et al Transfusion 2025). Other reviews have concluded that half of plasma transfusions lack a good indication.
A major U.S. critical care society issued formal guidance in March 2025 on the use of these blood products in critically ill patients. Here we review the recommendations and their evidence base.
PulmCCM is not associated with any professional society or medical journal.
When should fresh frozen plasma or platelets be transfused in the ICU, and when should coagulation abnormalities and thrombocytopenia be allowed to persist?
Plasma and Platelet Transfusions: Good Evidence Lacking
After screening 7,100 papers and reviewing 100 of them in detail, the authors identified only one randomized trial and 15 observational studies worth parsing for insights.
Given the clinical importance of the issue, this was itself striking.
They then used a modified Delphi technique (iterative surveys, discussions, and re-ratings of items) to come to a consensus on each topic.
This produced a list of suggestions (“conditional recommendations” based on very low-quality evidence).
Default Restrictive Approach Urged
As a top-line recommendation, the authors stated that
“Given the known risks of blood product transfusion, and the limited data regarding the benefits from platelet or FFP transfusion, most patients will benefit from avoiding transfusion of these blood products.”
This aligns with the well-established less-is-more restrictive approach to red cell transfusion in most hospitalized patients (in or out of ICUs).
Guidelines on Red Cell Transfusion (Review)
Anemia is the norm among critically ill patients, who were historically transfused to normal or near-normal hemoglobin levels in the hope of optimizing their physiology and chances for recovery.
But there’s a big difference in the evidence base.
The red cell transfusion practice standards are derived from more than a dozen randomized trials in more than 15,000 patients, which showed neither a benefit nor harm of a restrictive approach to red cell transfusion in general ICU patients (relative risk 0.99):
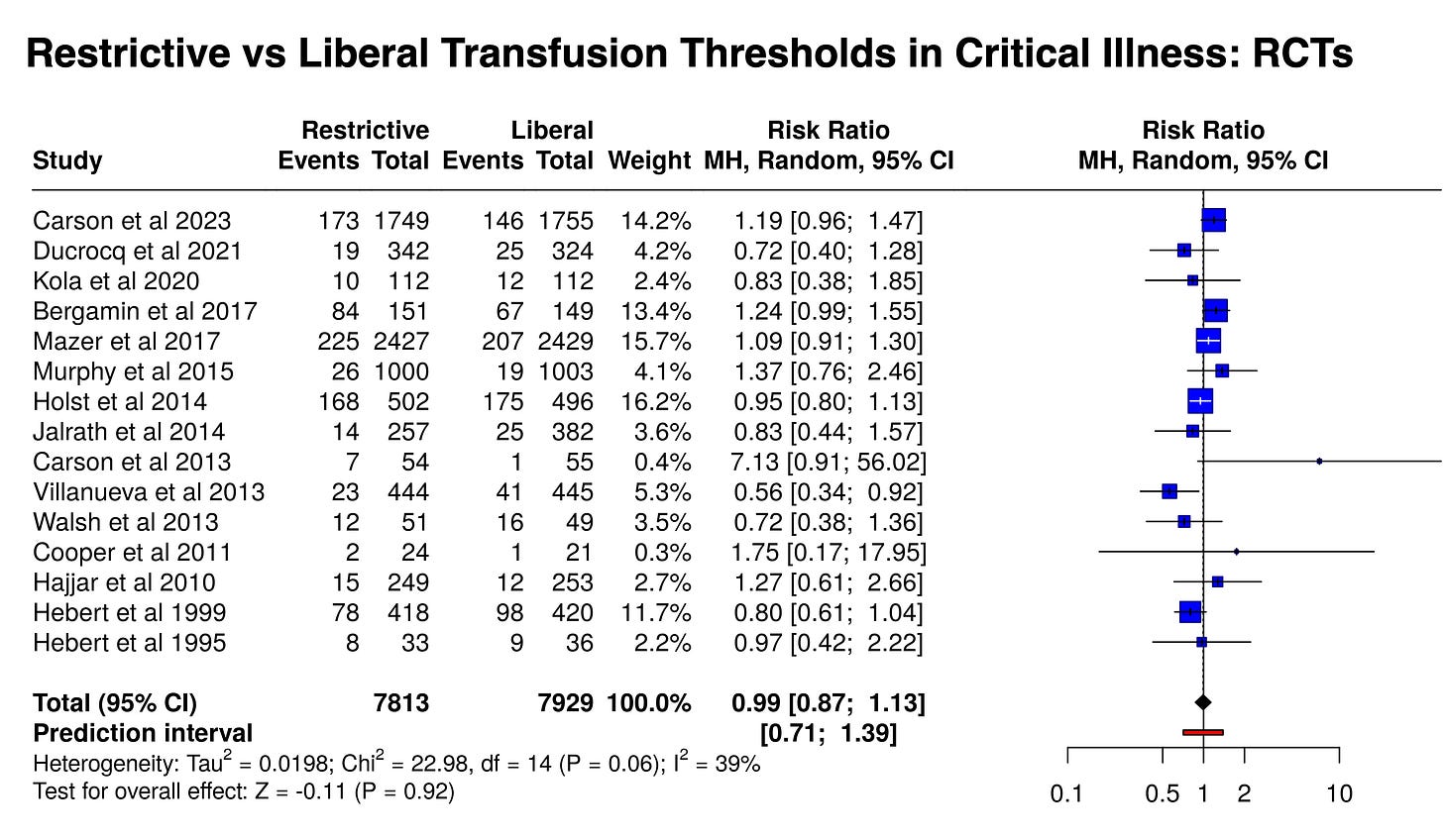
A much smaller sample size of ~1750 patients with active GI bleeding in three RCTs did suggest harms from a liberal transfusion strategy, i.e., benefits of a restrictive strategy:
From that comparatively enormous evidence base, we can strongly argue for a restrictive approach with red cells based on non-efficacy, but it’s hard to argue that most patients benefit from avoiding red cell transfusion.
With only one randomized trial and some observational data, is it justified to conclude that “most patients will benefit from avoiding transfusion” with FFP and platelets?
Before answering that, let’s first cut to the recommendations. (The original document is here.)
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.





