Issue #2: The Latest in Critical Care, 5/22/23
In The News
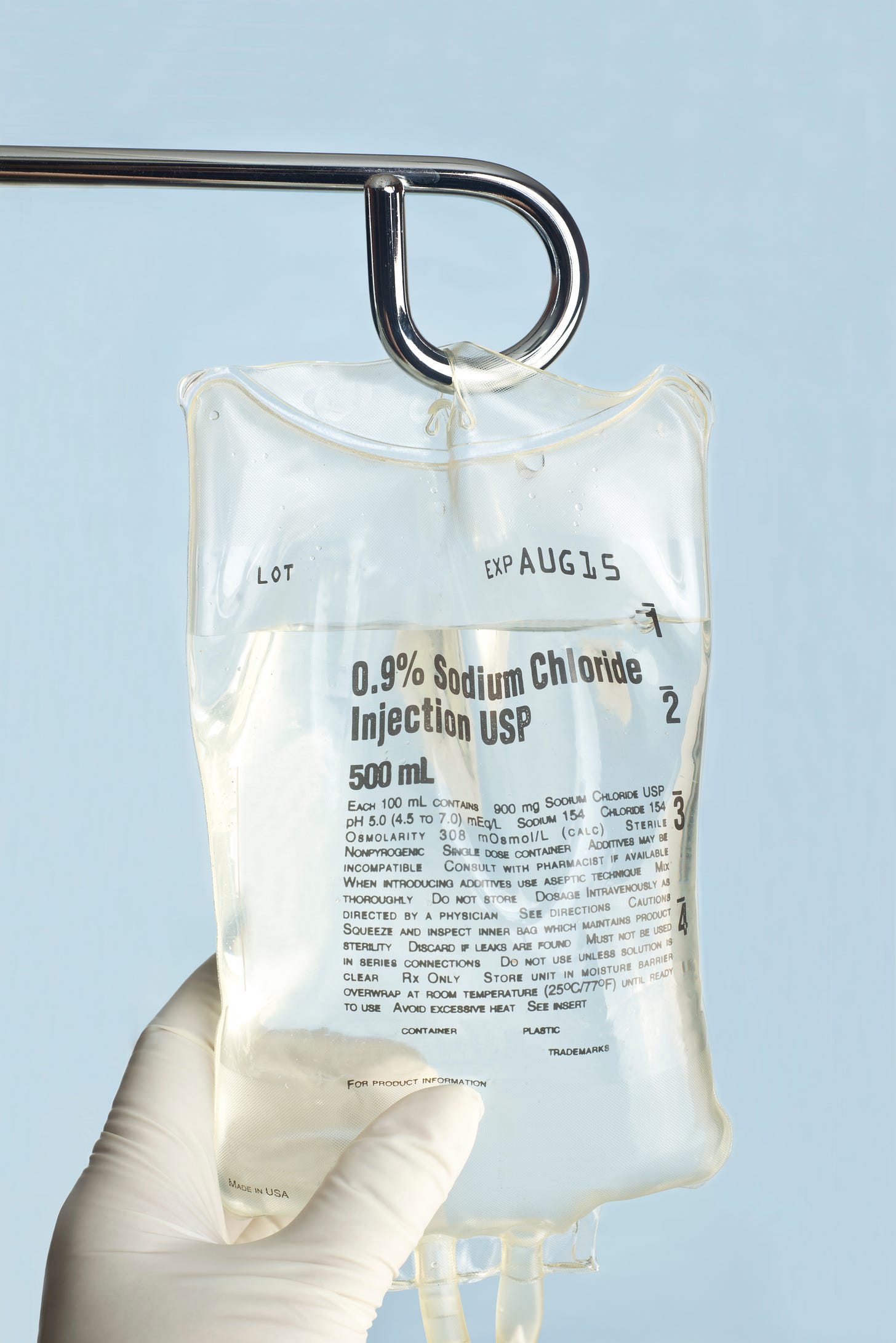
Drug shortages in the flawed generic drug supply chain are leading to overt rationing of vital drugs including cisplatin (a cornerstone of chemotherapy treatment for some cancers) and other serious conditions. Surveyed gynecologic oncologists recently reported chemotherapy shortages in 35 states (including at large cancer centers). The basic …
Keep reading with a 7-day free trial
Subscribe to PulmCCM to keep reading this post and get 7 days of free access to the full post archives.