The Latest in Critical Care: November 24, 2025
New mRNA vaccine for flu; steroids for CAP; IVC ultrasound for heart failure; transfusion in brain injury
Pfizer’s mRNA flu vaccine works better than the conventional shot
Because of the six-month production cycle for conventional influenza vaccines (which are still mostly produced in millions of inoculated fertilized chicken eggs each year), the flu strains to be targeted must be selected in February for the flu season that fall/winter (in the northern hemisphere).
The flu virus often mutates in the interim (antigenic drift), resulting in a poor match between the vaccine and the circulating strain. The virus also mutates inside the eggs, adding another source of mismatch. Poorly matched vaccines mean less protection and theoretically more illness and mortality.
Messenger RNA (mRNA) vaccines can be more rapidly developed and precisely targeted to specific viral particles, as the response to Covid-19 has demonstrated.
Pfizer recently released phase 3 data from its mRNA influenza vaccine, tested in 18,476 patients aged 18 to 64 in 2022-2023, half of whom got the mRNA shot and the other half a conventional inactivated quadrivalent influenza vaccine (control group).
The quadrivalent mRNA vaccine was about 35% more effective at preventing laboratory-confirmed influenza (57 vs 87 cases; CI ranging from 7% to 53% more effective).
However, it also produced significantly more fever (5.6% vs. 1.7%), local reactions (70% vs 43%), and systemic symptoms (66% vs. 49%).
Current vaccination practices are estimated to prevent ~1,000 deaths from influenza in the 18-64 age group (~6,500 —> ~5,500 deaths). This trial was not powered to detect a mortality benefit.
mRNA vaccines lack the long-term safety data available for conventional flu shots. In August 2025, the U.S. government halted $500 million in funding for mRNA vaccine development. Jay Battacharya, the NIH director, recently argued against any expansion of mRNA vaccine research by NIH, citing unresolved questions about their mechanistic effects such as how long the encoded proteins persist and where they are distributed in the body.
Jay Bhattacharya: Why the NIH is pivoting away from mRNA vaccines - The Washington Post
Covid vax continues to prevent disease in the post-pandemic era
Now that SARS-CoV-2 no longer fills ICUs with ventilated patients, the potential benefits of vaccination are less obvious. Concerns about the validity of epidemiologic methods and case definitions have led to uncertainty about how much of a health threat the virus continues to pose, and how much vaccination reduces that risk.
One of the main causes of uncertainty lies in the so-called “healthy vaccine effect,” in which healthier people tend both to get vaccinated against X disease more often, and to survive X more often, with their survival misattributed or overattributed to the vaccine rather than their general health. A large observational study got around that problem in an elegant way.
In the U.S. Veterans Affairs health system, 164,132 patients who got the Covid and influenza vaccines on the same day in 2024-2025 were compared to 131,839 patients who got the influenza vaccine only (many or most of whom presumably declined the Covid shot, which is offered at the same time).
By 6 months after the index vaccination, Covid-associated ED visits, hospitalizations, and deaths were all significantly lower among the group vaccinated against Covid. Risk reductions persisted across all age groups, but were highest in those aged 65 and older. The Covid vaccine effectiveness against the composite was estimated at 37%.
The Covid-associated death rate was 1.25% in the vaccinated group vs. 3.5% in the unvaccinated group. One in 29 veterans dying of Covid in six months in 2024-2025? Although this seems implausibly high and suggests some degree of bias, Covid may today cause more deaths indirectly by exacerbating other illnesses rather than directly by ARDS, myocarditis, etc. The large cohort and impressive design of the study are convincing that the Covid mRNA vaccine still prevents serious illness and deaths, especially in older adults.
More evidence for benefits of steroids in community-acquired pneumonia
Among 2,180 patients in Kenya admitted to 18 hospitals with a diagnosis of community-acquired pneumonia, those randomized to receive oral corticosteroids had improved survival at 30 days (22.6% vs. 26%). They were medical ward patients, as most of these hospitals did not have ICU capabilities. Pneumonia in these settings is diagnosed clinically, without chest radiography. Adverse events were almost nil. Guidelines advise systemic steroids for severe community-acquired pneumonia.
A Pragmatic Trial of Glucocorticoids for Community-Acquired Pneumonia. NEJM 2025
IVC diameter on ultrasound to guide diuresis in decompensated heart failure
Identifying volume overload is one of the most straightforward use cases for bedside ultrasound (i.e., POCUS). Inferior vena cava diameter is easily visualized and measured, and represents a potential standardized metric to guide decisions for diuretic therapy in heart failure.
The randomized CAVAL US-AHF trial (Burgos et al, American Heart Journal 2024) found that a strategy combining IVC measurements and lung ultrasound reduced “subclinical decongestion” over usual care, among 60 patients admitted with acute heart failure. Ultrasound markers for volume overload (B-lines on lung ultrasound and IVC diameter/collapsibility) dramatically improved in patients in the ultrasound arm, and a reduction in heart failure readmissions or urgent visits (13% vs 36%).
That trial was at a single center in Buenos Aires, Argentina.
The CAVA-ADHF-DZHK10 trial then enrolled 388 patients admitted for decompensated heart failure at multiple centers in Germany, of whom 327 were analyzed by intention to treat.
Those who were randomized to IVC diameter-guided decongestion had no greater improvement in their NT-pro-BNP levels than usual care patients, nor in the secondary outcomes tested. In contrast to the CAVAL US-AHF trial, lung volumes were not used to guide decongestion.
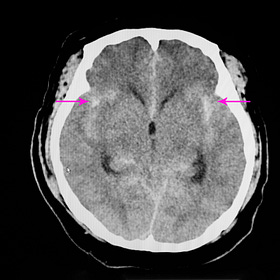
Liberal vs restrictive RBC transfusion in brain-injured patients: meta-analysis
Studies of red cell transfusion thresholds for “acute brain injury” tend to lump together patients with strokes, traumatic brain injuries, and sometimes anoxic-hypoxic encephalopathy. In this heterogeneous group, liberal transfusion to higher hemoglobin targets (e.g., 9 to 10 g/dL) appears to lead to better outcomes than restricting transfusion.
Blood transfusion targets in acute brain injury: Review (Updated)
This review was first published in October 2024; it is updated here with important new results from the SAHARA trial (English et al NEJM 2024), with a series of (rough) meta-analyses of recent data. -Ed.
A new meta-analysis of six randomized trials (n=2,497) concluded that a liberal transfusion strategy led to higher rates of favorable neurologic outcomes (RR 0.89), and trends toward improved mortality and length of stay.
When TBI patients (n~1,400) were analyzed as a separate subgroup, similar results were found to the overall population. Significant heterogeneity remained, though, with caution advised in interpreting the results.