The Real-World Boards: Question #16
An elderly man has abrupt respiratory distress after a stroke
These are the Real-World Boards. As in the real world, there may be no single “right” answer, and you are only competing against yourself. Upgrade to the Lifelong Learner level for full access to all the questions and unlimited CME credits with an included Learner+ account.
You are called to the bedside of a 75-year-old man in the ICU. He was admitted yesterday with a large ischemic stroke and was treated with thrombolytics and thrombectomy. He has been encephalopathic with left-sided weakness, but had no trouble breathing and was on room air earlier that day. His BMI is 35.
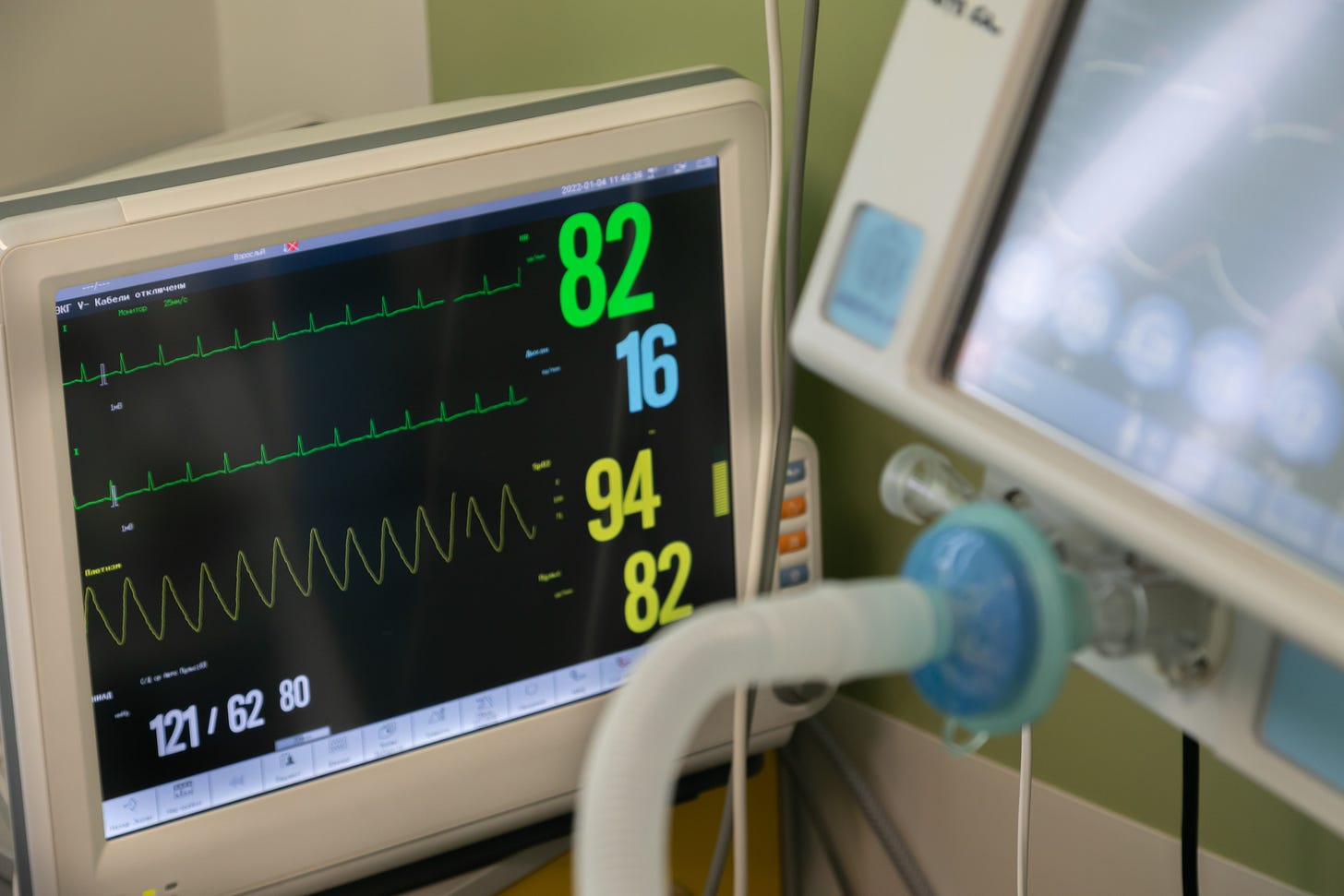
He was found by the RN in respiratory distress, gasping and using accessory muscles after an episode of emesis. His SpO2 was 83% on 5 L/min oxygen before you arrived. SpO2 is now 95% on FiO2 100% with high-flow nasal cannula oxygen, but his work of breathing is not reduced.
You decide to intubate.