The Real-World Boards: Question #19
A 68-year-old man with multiorgan failure and declining urine output
These are the Real-World Boards. As in the real world, there may be no single “right” answer, and you are only competing against yourself. Upgrade to the Lifelong Learner level for full access to all the questions and unlimited CME credits with an included Learner+ account.
You are caring for a 68-year-old man who weighs 70 kg who developed acute kidney injury associated with sepsis in the ICU. He was mechanically ventilated on hospital day 1 for acute hypoxemic respiratory failure and presumed pneumonia/ARDS, now with a P/F ratio of 225. He is receiving norepinephrine at 0.2 mcg/kg/min.
Serum creatinine rose from 1.2 mg/dL on admission to 3.8 mg/dL currently, and urine output has fallen to 550 mL in the past 24 hours (~0.3 mL/kg/hr), with a net positive 7-liter fluid balance, despite receiving furosemide 40 mg IV bid. He has pitting edema in all extremities on exam. Chest film shows persistent bilateral infiltrates, unchanged.
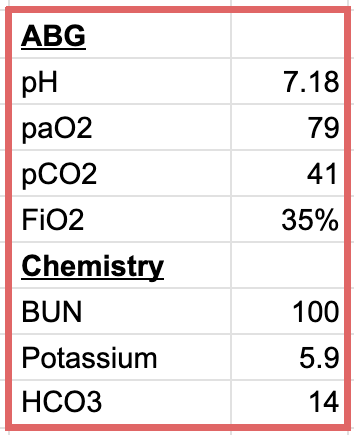
Labs include:
The nephrologist asks if you would like her to start renal replacement therapy.
The timing of initiating renal replacement therapy for AKI in critical illness has been tested in several large, multicenter, randomized trials. ICU patients with borderline indications for dialysis were randomized to either immediate RRT or delaying RRT until prespecified criteria were met (persistent oliguria, pulmonary edema, hyperkalemia, etc).