The Real-World Boards: Question #21
A 48-year-old man with ESRD and a new pleural effusion
These are the Real-World Boards. As in the real world, there may be no single “right” answer, and you are only competing against yourself. Upgrade to the Lifelong Learner level for full access to all the questions and unlimited CME credits with an included Learner+ account.
A 48-year old man with end-stage renal disease on chronic hemodialysis underwent successful routine “permcath” tunneled dialysis access placement two days ago.
You are called to his bedside for respiratory distress. He is in mild distress with tachypnea and a new 3 liters/min oxygen requirement. He describes right sided chest pain. Blood pressure is 126/70 (from 166/90), heart rate 111/min, respirations 22/min, SpO2 96%, and afebrile. Hemoglobin was 9 g/dL and is now 6 g/dL. A transfusion of two units of packed red cells has been ordered stat.
A chest film after the procedure two days ago was unremarkable. A new chest radiograph is obtained.
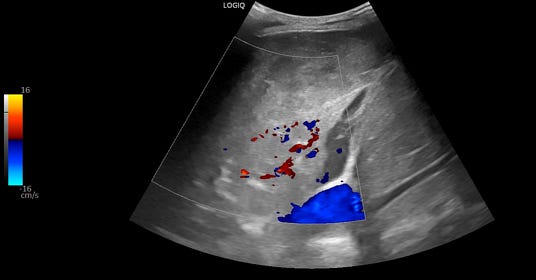
A bedside thoracic ultrasound is also obtained. The right thorax showed:
The patient has a new large pleural effusion with borderline hemodynamic instability and worsening hypoxemia.
Ultrasound shows a collapsed right lower lobe with hyperechoic material in the right hemithorax.
With a significant drop in hemoglobin and a new large right-sided pleural effusion ipsilateral to a recently placed tunneled dialysis catheter in the subclavian vein, iatrogenic hemothorax is a likely diagnosis.