The Real-World Boards: Question #22
A 70-year-old woman with the sudden onset of chest pain and dyspnea
These are the Real-World Boards. As in the real world, there may be no single “right” answer, and you are only competing against yourself. Upgrade to the Lifelong Learner level for full access to all the questions and unlimited CME credits with an included Learner+ account.
A 70-year-old woman presents to the emergency department after experiencing the sudden onset of chest pain and dyspnea about two hours ago. When she arrived by EMS 30 minutes ago, you see she was normotensive (BP 144/87), in sinus tachycardia with a rate of 117, with SpO2 95% breathing ambient air, 18 breaths/min.
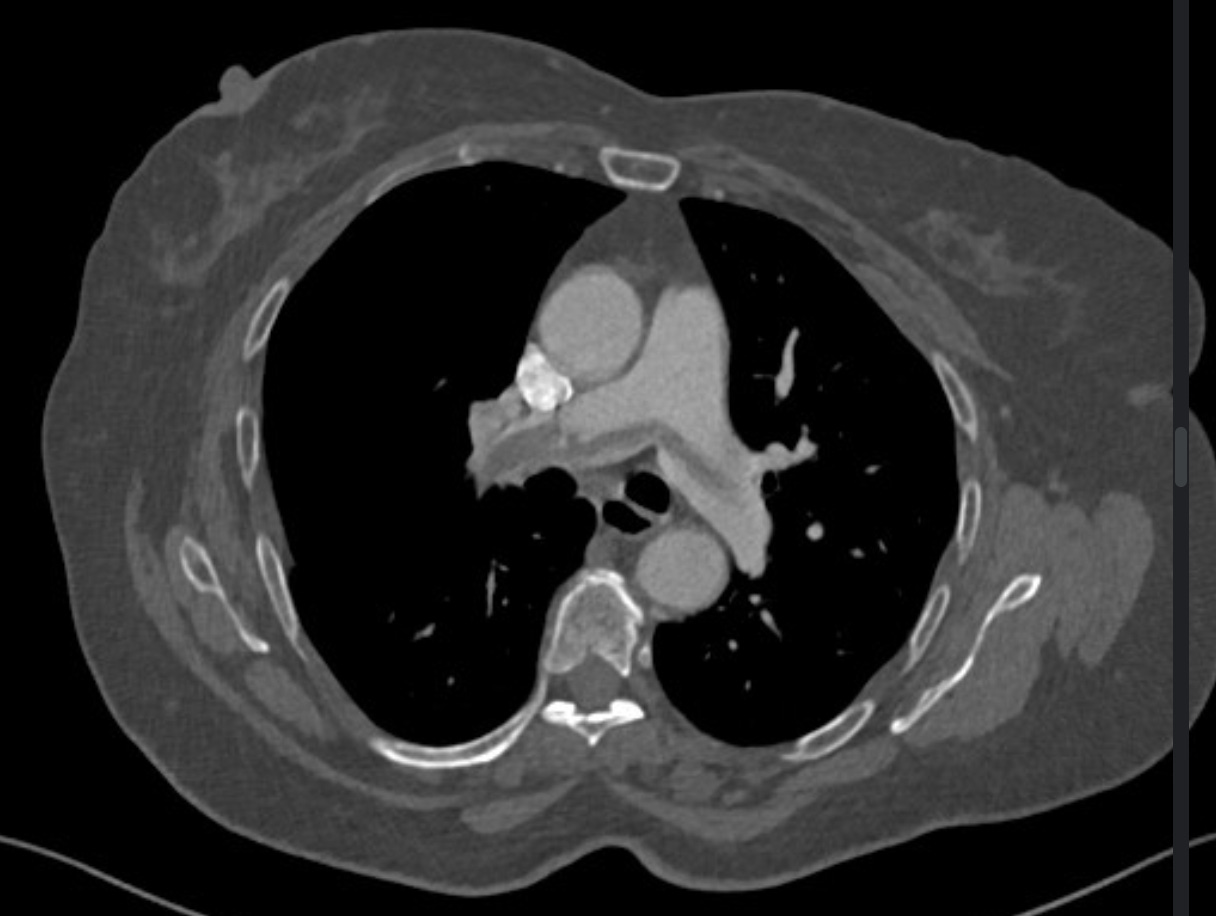
A CT-angiogram was performed:
The patient care technician shows you the most recent vitals: BP 101/62, HR 129, SpO2 90%, RR 24/min (similar when repeated 20 minutes later).
Hemodynamically unstable (so-called massive) pulmonary embolism is defined as either systolic blood pressure <90 mmHg or a drop in systolic BP of ≥40 mmHg from baseline for more than 15 minutes (and/or shock or cardiac arrest).
Along with supplemental oxygen, cautious intravenous fluid boluses for preload, and vasopressors if needed, short-acting intravenous unfractionated heparin is usually advisable over enoxaparin for patients who might require reperfusion therapy.