The Real-World Boards: Question #26
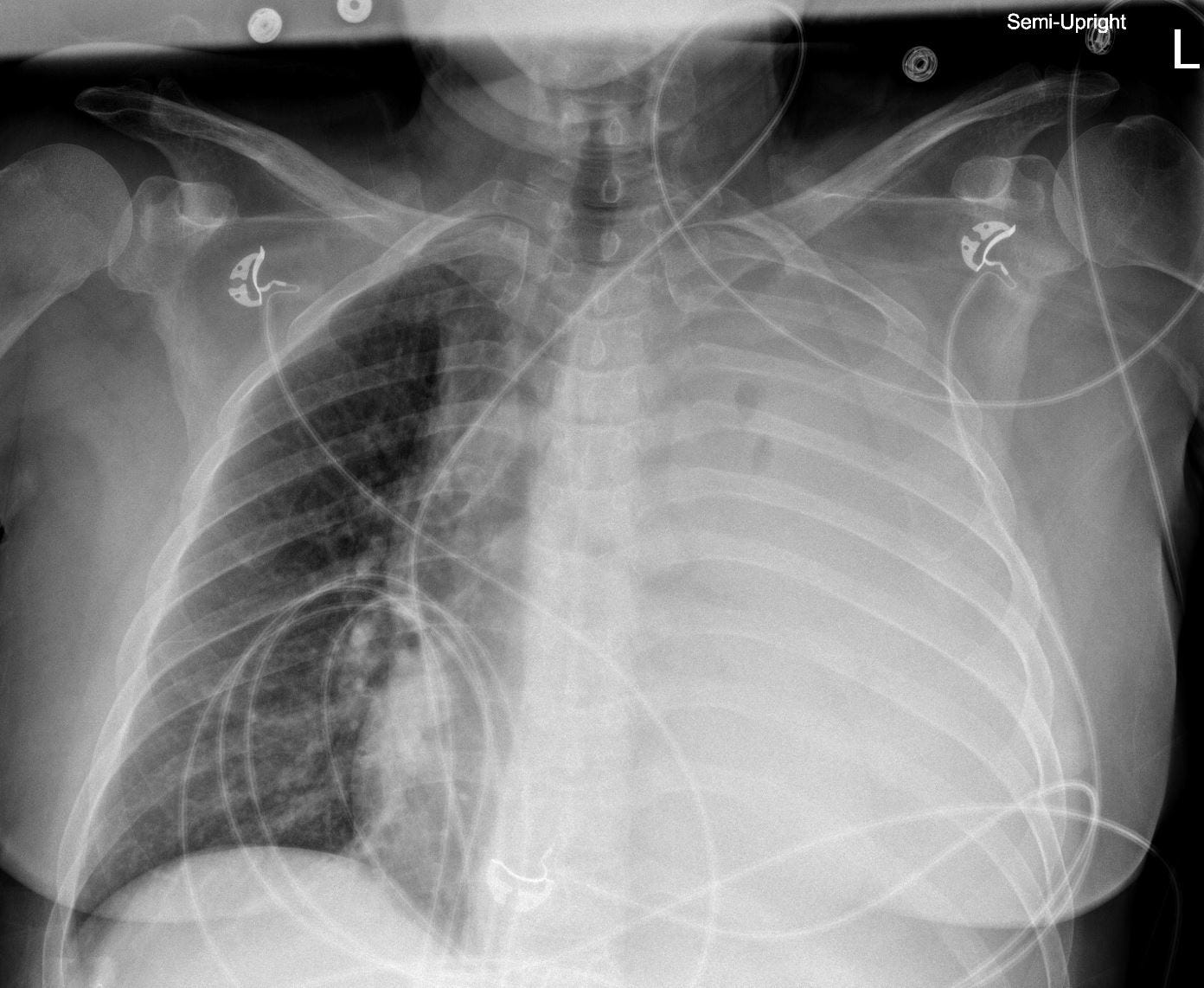
Wow, that's a big effusion
These are the Real-World Boards. As in the real world, there may be no single “right” answer, and you are only competing against yourself. Upgrade to the Lifelong Learner level for full access to all the questions and unlimited CME credits with an included Learner+ account.
A 54-year-old man with a long history of ongoing alcohol abuse and dependence was admitted to the medical ward a week ago with encephalopathy. He was treated for alcohol withdrawal delirium with symptom-directed therapy.
His encephalopathy did not improve, and four days ago he was found to be poorly responsive and breathing rapidly and shallowly with a new 5L/min oxygen requirement, unchanged pulse 110/min, and unchanged BP 90/60.
Chest film (4 days prior):
He was electively intubated, and a chest tube was placed with 2 liters of straw-colored fluid evacuated immediately.
The pleural fluid had an LDH of 80 U/L (serum: 220), protein 1.2 g/dL (protein: 4.2), culture-negative, with 120 polymorphonucleocytes per μL.
Follow-up chest films have shown only a small effusion, but the chest tube output has been more than one liter daily.
Abdominal ultrasound showed cirrhosis with a small amount of ascites not amenable to paracentesis. Lactulose was begun per NG tube. He has been treated with empiric antibiotics. Diligent fluid resuscitation has replaced the chest tube losses with crystalloid and occasional albumin doses, maintaining hemodynamics and renal function.
Chest tube suction is interrupted, and a large effusion reaccumulates within one day without tamponade physiology.
He marginally passes spontaneous breathing trials from a respiratory standpoint, and encephalopathy has improved. Extubation has been deferred pending decisions about the effusion.