The Real-World Boards: Question #8
Coagulation abnormalities arise in a 76-year-old woman with sepsis and shock
These are the Real-World Boards. As in the real world, there is often no “right” answer, and you are only competing against yourself. Upgrade to the Lifelong Learner level for full access to all the questions and unlimited CME credits with an included Learner+ account.
You are treating a 76-year-old woman in your ICU with sepsis due to E. coli bacteremia. She is mechanically ventilated and receiving moderate-dose norepinephrine and vasopressin. On day 4, you note oozing from her central line site. Mottling is present on her lower extremities, with doppler pulses present.
Labs show:
Disseminated intravascular coagulation is an often-lethal complication resulting from sepsis, cancer, trauma, obstetric complications, and many other less common causes.
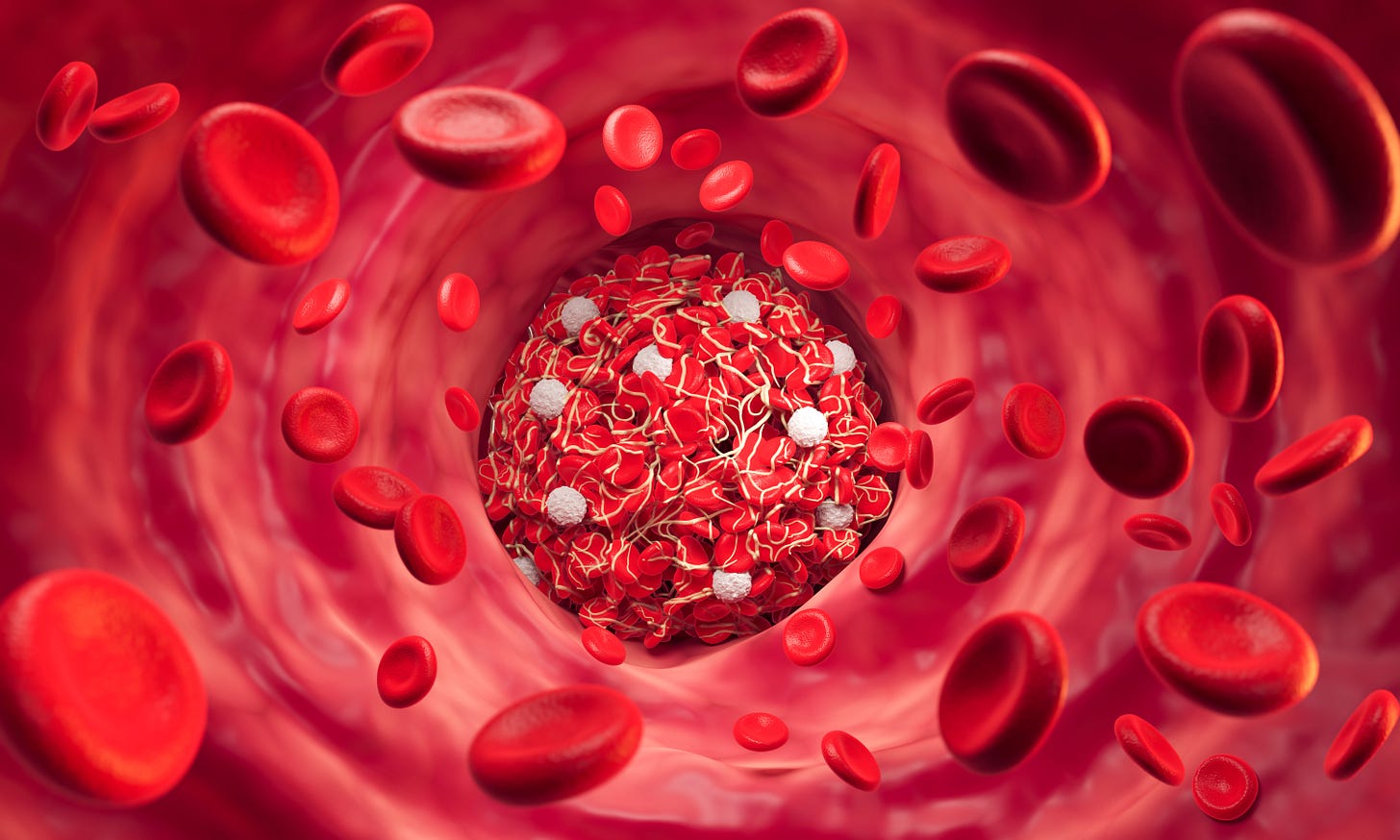
In DIC, circulating blood is exposed to tissue factor or other procoagulant substances that are normally sequestered in cells. Recent research suggests that dying neutrophils expel DNA into the bloodstream, where they form weblike structures called “neutrophil extracellular traps”. These highly procoagulant complexes appear to be a major contributor to the development and progression of acute DIC.
Diffuse microthrombi then develop, consuming clotting (and anti-clotting) factors and platelets, potentially causing multi-organ injury. As DIC worsens, a “consumption coagulopathy” develops, increasing the risk for bleeding. Fibrinogen is further depleted while producing fibrin degradation products and D-dimers. Organ injury occurs through deposition of microthrombi or bleeding.
Sepsis-related DIC has a high mortality (~40%), which has remained high despite improvements in sepsis mortality overall.
Diagnosis of DIC
The DIC diagnosis is made on the basis of compatible clinical and laboratory findings. CBC, PT/INR, aPTT, D-dimer, and fibrinogen are commonly checked and reveal a coagulopathy. Peripheral blood smear often shows scant schistocytes and helmet cells consistent with a microangiopathic hemolytic anemia, but not as pronounced as in more fulminant MAHAs like thrombotic thrombocytopenic purpura.
A validated scoring tool by the International Society on Thrombosis and Hemostasis (ISTH) can increase confidence in the diagnosis of DIC. Higher scores predict mortality, and serial testing is suggested.
Overt vs. Non-overt DIC
Overt DIC represents clinically recognizable DIC, with coagulation abnormalities, thrombocytopenia, and oozing or frank bleeding. An ISTH score ≥5 is consistent with overt DIC.
Non-overt DIC is compensated or early DIC, sometimes with elevated D-dimer as the only obvious abnormality. Regular monitoring of appropriate lab values is advisable in suspected non-overt DIC.
Management of DIC
Like sepsis, the scale and multiplicity of systemic derangements in DIC have proved largely impervious to pharmacological efforts to terminate the disorder’s complex processes. Specialized anticoagulant therapies have shown some suggestion of benefit in randomized trials, but are not endorsed in international guidelines.
Treating the underlying cause (e.g., sepsis, trauma, retained products of conception, etc.) and supportive ICU-level care are cornerstones of acute DIC management.