The Latest in Critical Care: September 22, 2025
Organ procurement shutdown; New antibiotic for S. aureus; MAP targets in spinal cord injury; ETCO2 in cardiac arrest; "ICU delirium" and driving after discharge
Dalbavancin not better than vancomycin for S. aureus bacteremia
Dalbavancin is a long-acting intravenous agent with a long half-life of 14 days and potent in vitro activity against S. aureus, including methicillin-resistant strains (MRSA). This has made it tempting to use for patients with complicated infections that require long-term treatment, because dalbavancin can be given weekly, eliminating the need for long-term intravenous access.
Dalbavancin is FDA-approved to treat skin and soft tissue infections caused by Staphylococcus aureus. It has also been successfully used off-label to treat S. aureus bacteremia, but treatment failures were reported in complicated infections (e.g., osteomyelitis, endocarditis, etc).
Among 200 adults with complicated S. aureus bacteremia, dalbavancin had equal clinical efficacy to vancomycin (73% vs 72%), in the DOTS randomized trial. Dalbavancin did not achieve superiority in the complicated composite endpoint comprising multiple outcomes.
—Turner et al, “Dalbavancin for Treatment of Staphylococcus aureus Bacteremia: The DOTS Randomized Clinical Trial,” JAMA 2025
See also:
HHS forces Miami organ procurement organization to shut down
The U.S. government has cut ties with Life Alliance Organ Recovery Agency in South Florida, effectively excluding the organ procurement organization from participating in organ harvesting and donation. The OPO (along with others) was mentioned in the New York Times’s earlier reporting as having engaged in questionable ethical practices when securing organ donations after circulatory death (as opposed to donation after brain death):
“In 2023, doctors at a Florida hospital withdrew life support from a patient although he was crying and biting his breathing tube, according to two Life Alliance employees. The man died, and his organs were removed,” the Times reported.
The termination follows a years-long investigation by the federal government into organ procurement practices. The Miami-based organ procurement organization can appeal the decision.
“Organ Transplant Group Faces Shutdown After Safety Problems”, New York Times, September 18, 2025
See also:
Transplant surgeons allege corruption and mismanagement in organ transplant system
Critics of the shortcomings of the organizations responsible for organ donation and transplantation launched a surprise attack in a congressional subcommittee hearing this week.
Spinal cord-injured patients did not benefit from higher MAP targets*
*in an underpowered trial
For spinal cord-injured patients, augmenting blood pressure (with vasopressors, if necessary) to maintain high-normal mean arterial pressure is a standard practice recommended by neurosurgery guidelines. However, it’s based on physiology and possibly confounded observational evidence, not randomized trial data.
Among 92 adults with spinal cord injury, those randomized to higher mean arterial pressure targets (>85-90 mm Hg) had similar neurologic outcomes as those randomized to conventional MAP targets (>65-70 mm Hg).
The trial was underpowered to confidently rule out any clinically significant difference, because of slow enrollment, the Covid-19 pandemic, and financial constraints. Only 38 patients completed the 6-month follow-up. There was significant overlap (inadequate separation) between groups in actual BP targets achieved.
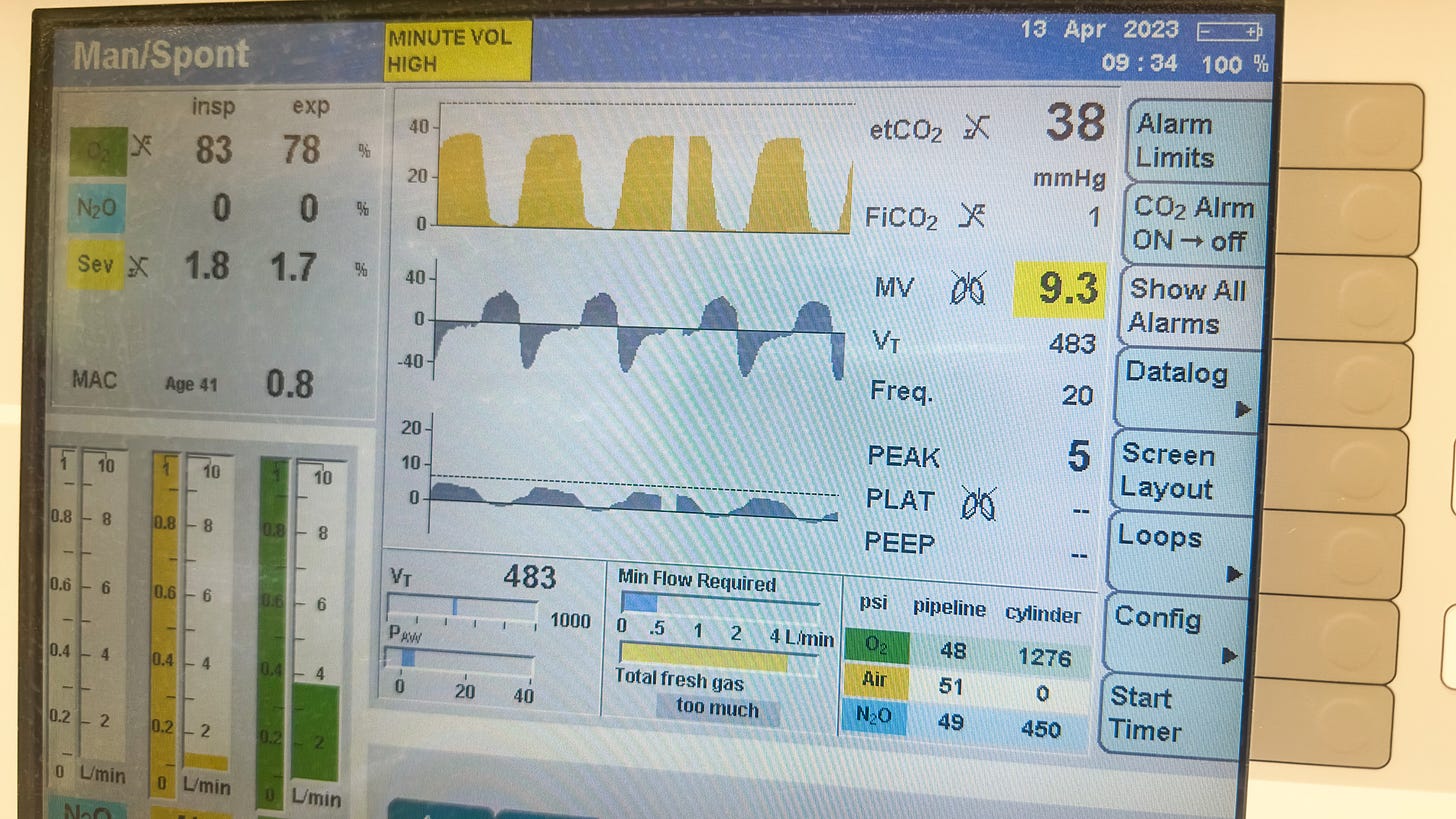
ETCO2 of questionable reliability in supraglottic airways, in PART post hoc
The Pragmatic Airway Resuscitation Trial (Wang et al, JAMA 2018) found that out-of-hospital cardiac arrest patients who were randomized to endotracheal intubation by first responders had significantly lower 72-hour survival than those who received supraglottic airways (e.g., iGel) as the first attempted airway.
That was undoubtedly in part because only half the patients randomized to intubation were successfully intubated; the other half were rescued with SGAs after repeated failed intubation attempts.
In a follow-up post hoc study, end-tidal CO2 was found not to differ at various time points of resuscitation, regardless of the device used. However, ETCO2 trends with an ET tube in place were much more predictive of ROSC than those with an SGA in place (which were in turn confounded by the inclusion of many patients who had failed ET intubation), precluding any conclusions about physiologic equivalency between the two advanced airway strategies.
PART trial, Wang et al, JAMA 2018
“ICU delirium” did not predict declines in driving skill post-discharge
Patients discharged after critical illness reported driving less than before their illness, and avoiding nighttime driving, driving in the rain, and parallel parking. About one in seven reported a driving accident in the months after discharge. However, patients who were diagnosed with “ICU delirium” were no more likely to experience a decrease in driving skill or frequency, compared to patients not flagged as delirious.
Physiology Flashback!
ICU Physiology in 1000 Words: Venous Excess & the Myth of Venous Return
Jon-Emile S. Kenny MD [@heart_lung]







I am baffled at this rate of success at first intubation attempt 😮